Modern senior living EHR platforms have become essential tools for operators who manage many assisted living and memory care communities. Regulations keep changing and surveys continue to increase. As COOs, we face steady pressure to maintain strong documentation, avoid compliance issues, and protect every facility license in the portfolio. Current EHR technology supports these goals by guiding staff workflows, improving accuracy, and giving us clear oversight across all locations.
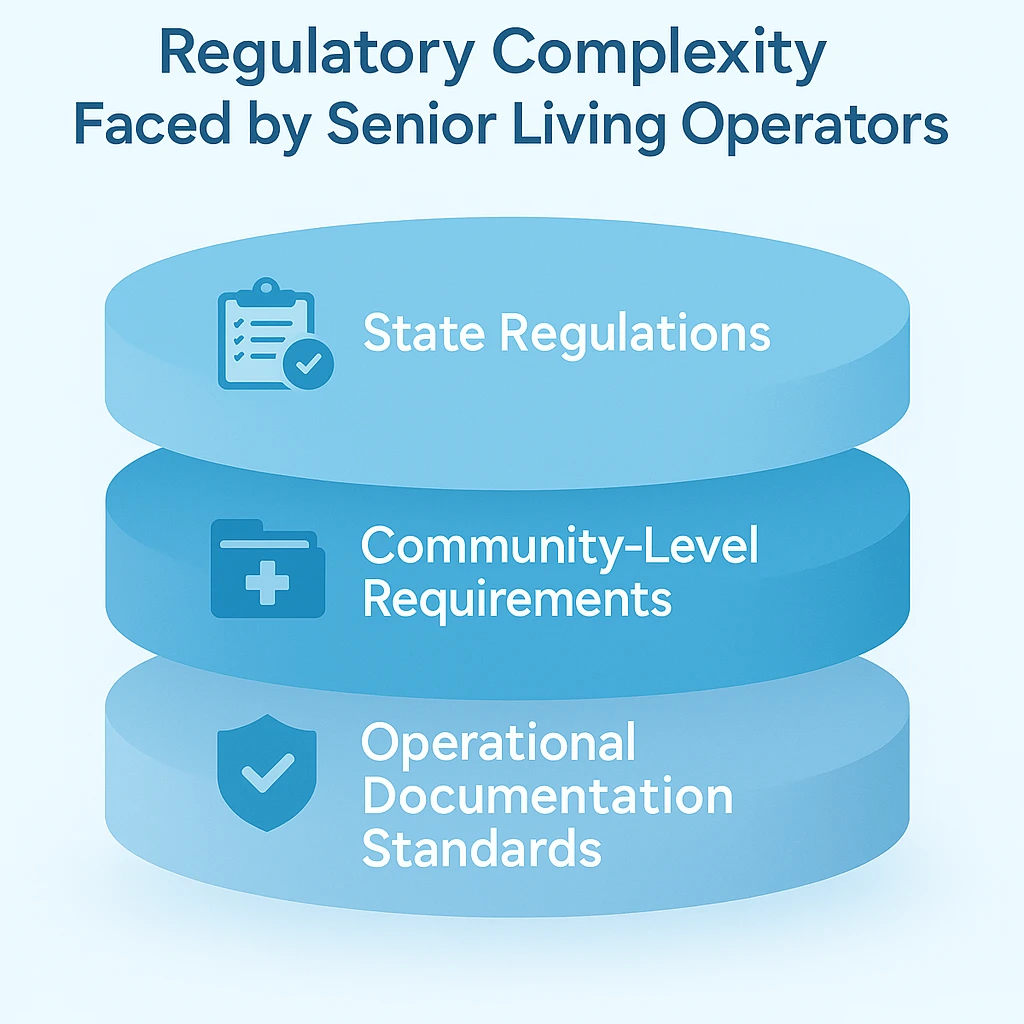
Senior living rules are complex because each state writes its own standards. When we operate in more than one state, we must follow several rule sets at the same time. These rules affect assessments, care plans, medications, staffing, and incidents (1)(2). Without a consistent system, documentation varies from site to site and the chance of mistakes grows.
This challenge increased after the pandemic. Many states added surveys, tightened expectations, and asked for faster access to records (3). Surveyors now expect complete documentation that is easy to pull at any moment. Paper charts and older software often cannot meet this requirement. Many older systems also do not include clear audit logs, so it becomes harder to explain what happened and when.
High staff turnover adds more pressure. Annual turnover rates for direct care workers often pass fifty percent (4). New hires and agency staff may struggle with manual documentation. A good EHR provides structure, prompts, and required fields. These tools help staff complete tasks correctly and consistently.
The most helpful part of a modern senior living EHR is its ability to keep documentation uniform. When all caregivers record activities, medications, incidents, and reassessments using the same method, we reduce the risk of uneven practices that lead to survey findings (5). Fewer tools, forms, and spreadsheets mean fewer errors.
The core value of a modern senior living EHR is its ability to standardize documentation across a multi-community portfolio. This creates a stable foundation for compliance across the entire organization.
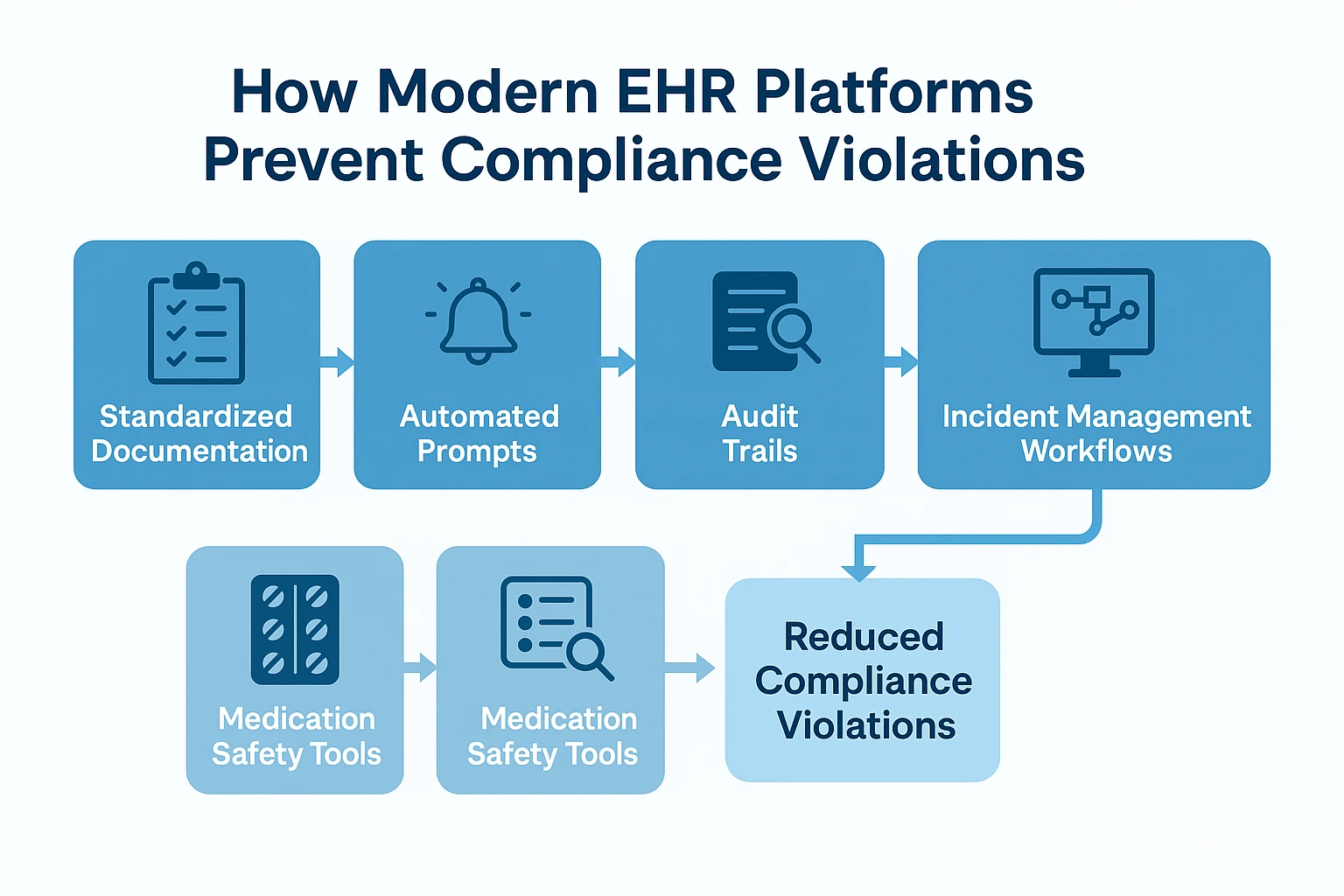
Automation adds more support. Modern systems remind caregivers when service plans are due. They flag medication problems and prompt staff to record important details in memory care (6). These reminders reduce missed steps and incomplete notes.
Audit trails also matter. Modern EHRs record who made each entry, the time of entry, and any changes. During a survey or complaint review, these details show clear evidence of care delivery (7). Older systems and paper records often cannot provide this level of detail.
Medication management improves with eMAR tools, barcode checks, pharmacy links, and real-time alerts (8). These features reduce documentation gaps and missed doses. They are especially helpful for memory care residents who often have frequent medication changes.
Incident reporting also becomes more reliable. Many states require reports within a certain number of hours. An EHR can guide caregivers through the first report, track follow up, and alert supervisors (9). This lowers the chance of late or incomplete reporting.
Infection control has become more important. EHRs help track symptoms, exposure risks, screening results, isolation steps, and PPE use. When we can see this information across all communities, we can respond more quickly and prove that we followed required practices.
Staffing needs are changing in many states. Regulators expect staffing levels to match resident needs. EHRs can show care intensity and highlight where staffing may be too low (10). This helps COOs plan schedules and explain decisions with clear data.
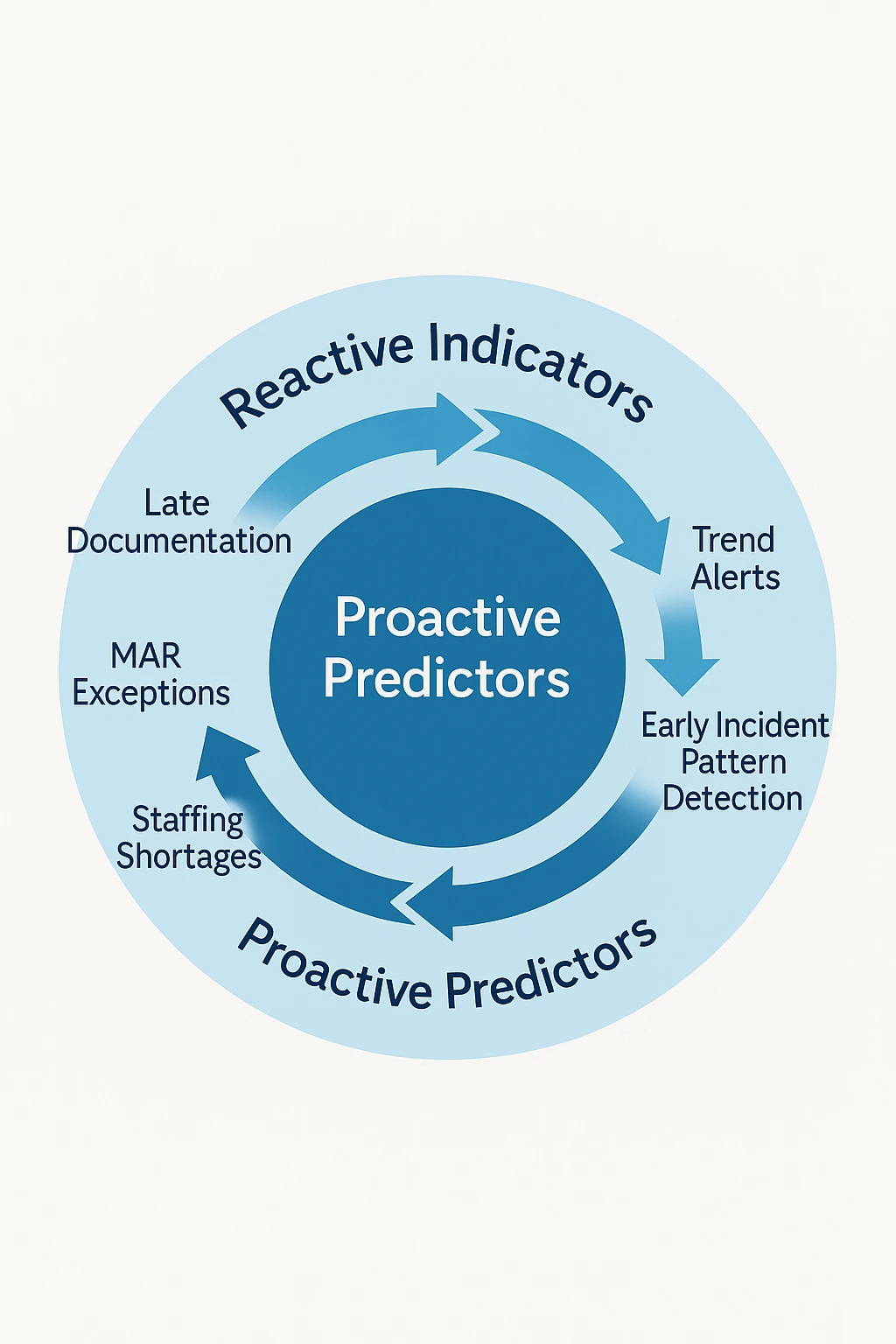
A strong EHR also gives COOs real visibility across the entire portfolio. We can see which buildings are late with service plans, falling behind on documentation, or showing rising medication problems. This helps us step in early.

Dashboards help identify which communities need extra support. For example, a building may have more behavioral incidents, repeated medication issues, or infection control gaps. Benchmarking also helps us compare performance between sites and catch patterns that deserve more focus.
Early warning signals matter. EHR analytics can highlight repeated late documentation, frequent MAR exceptions, or clusters of falls. When we catch these trends early, we can respond before they become compliance findings or threats to licensure.
Survey readiness improves with a strong EHR. Teams can quickly pull complete records, including assessments, service plans, medications, and incidents. This reduces stressful interviews and helps avoid mixed responses.
Mock audits are easier to run when records are digital. Clinical and compliance teams can review key areas in advance (11). Routine audits often lead to better survey outcomes.
Centralized digital records also strengthen legal defense. In many liability cases, problems arise when documentation is missing or inconsistent (12). Standardized records make it easier to show what care was provided.
Memory care programs benefit as well. These settings require detailed notes about behavior, cognition, and care strategies. Templates support thorough tracking and reduce gaps that regulators often check (13).
Compliance problems can cause real financial strain. Citations can lead to correction plans, training, monitoring, fines, or damage to a community’s reputation. In severe cases, they can threaten community licenses. A single license represents significant value, so protecting them is essential.

EHR systems also help with accountability. When tasks are missed, supervisors can see the issue quickly. Alerts help leaders follow up before small issues grow (14). This leads to more stable care and better satisfaction for residents and families.
In the end, EHR platforms support the essential work of protecting community licenses. They help reduce compliance risks, improve documentation, and give COOs the information they need to maintain safe and effective operations across all buildings.
As regulations keep evolving and documentation expectations increase, operators with strong EHR systems will be better prepared to meet these demands and provide consistent care. We can use these insights to check whether our current system has the level of structure, clarity, and visibility needed for long-term success.
References
- National Center for Assisted Living (NCAL). “Assisted Living State Regulatory Review.”
- U.S. Centers for Medicare & Medicaid Services (CMS). “State Operations Manual.”
- U.S. Department of Health and Human Services (HHS). “COVID-19 Nursing Home Data and Oversight Reports.”
- PHI National. “U.S. Care Workforce Turnover Statistics.”
- LeadingAge & Argentum Regulatory Studies.
- State Survey Agency Annual Deficiency Reports.
- U.S. Office of Inspector General (OIG). “Audit and Investigation Documentation Standards.”
- Institute for Safe Medication Practices (ISMP). “Medication Error Reports in Long-Term Care.”
- State Departments of Health, Incident Reporting Requirements.
- Assisted Living Staffing Regulations, various states.
- Joint Commission and state-level mock survey data.
- Senior living liability and litigation trend reports.
- Alzheimer’s Association Dementia Care Practice Guidelines.
- National Quality Forum (NQF), long-term care quality studies.
Disclaimer:
This article provides general information for educational purposes and does not constitute legal, regulatory, financial, or compliance advice. Assisted living and memory care regulations vary widely by state and may change without notice. Requirements related to HIPAA, cybersecurity, documentation, and electronic health records depend on your organization’s structure, payer relationships, billing methods, and operational practices.
You should consult qualified legal counsel, regulatory specialists, or state licensing authorities to determine the specific obligations that apply to your communities and to verify how the guidance in this article relates to your organization’s compliance responsibilities.







.jpeg)