Introduction: Why Documentation Quietly Hits Your P&L
If you oversee three to ten assisted living and memory care communities, you already track the big numbers: labor, occupancy, agency spend, and NOI. Documentation usually sits in the background. It feels like how care gets recorded, not a real cost lever.
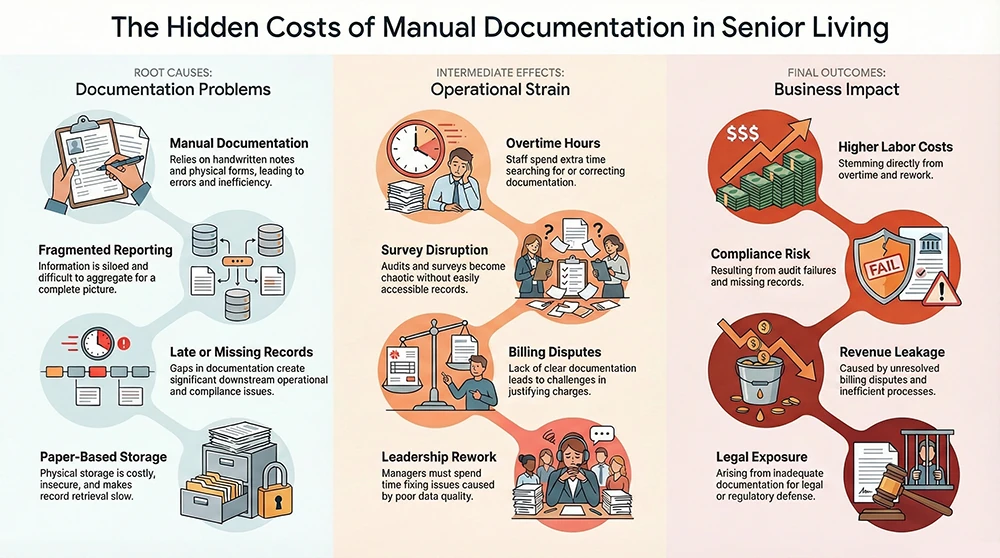
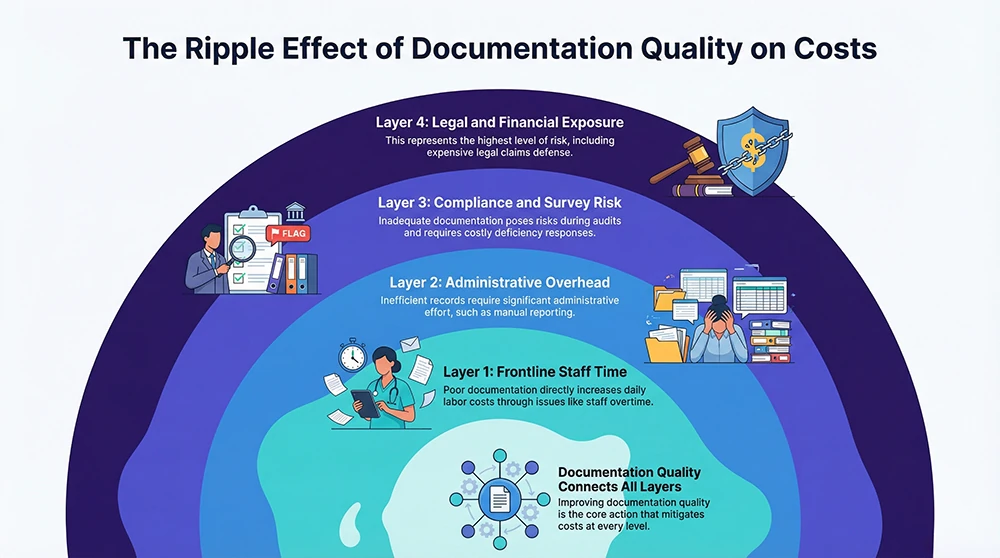
In practice, documentation touches everything you pay for. When charting is slow or inconsistent, your team stays late to finish notes. When records are hard to find, leaders scramble during a survey. When an incident happens, you spend hours rebuilding the story from scraps. And when billing questions come up, your team loses time proving what was done and why. Those are direct costs. They show up as overtime, rework, delayed decisions, and higher risk.
Digitizing documentation and reporting, especially through a purpose-built assisted living EHR like the one described at Fynn’s senior living EHR platform, changes the daily math. You are not buying more technology. You are buying time back, reducing preventable disruption, and creating records that hold up when they matter most.
1. Labor Savings You Can Actually Feel in Daily Operations
Documentation Time Is Real Time You Pay For
In many care settings, nurses spend a large share of their work time on documentation and related record work, sometimes around a quarter of the shift in time-and-motion studies (1) (2). Even if your buildings are not nursing homes in the strict sense, the operational reality is similar. Documentation takes time, and time is labor cost.
You see the impact in small ways that add up fast. A caregiver finishes med pass and still has to find the paper MAR, correct a missed signature, and track down a supervisor for a clarification. A nurse spends the last hour of a shift closing loops on notes that should have been done earlier, then stays late to finish. Multiply those moments across a week, across staff, across communities.
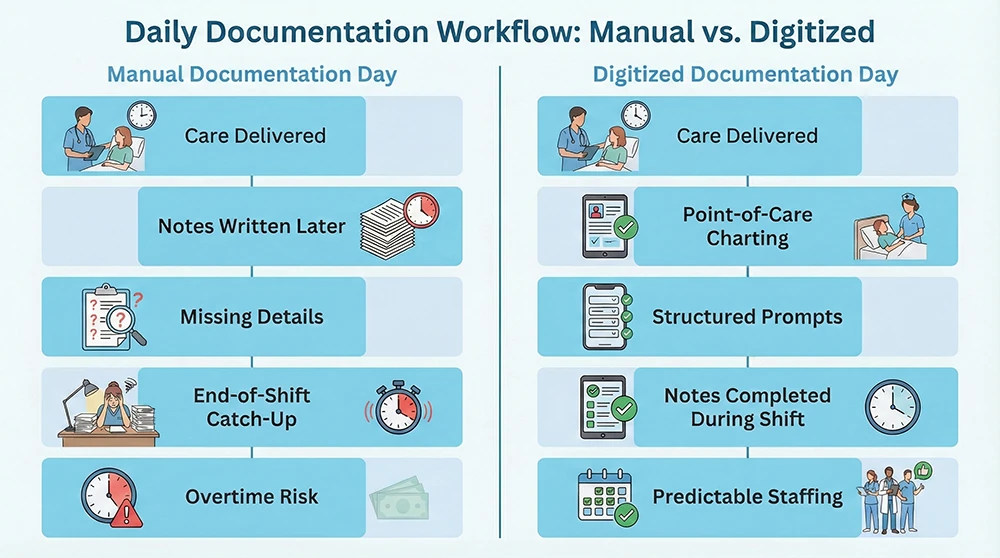
Digitized Charting Reduces Rework and End-of-Shift Pileups
When documentation is digitized inside a senior living EHR, you can shift charting closer to the point of care. That matters because most rework comes from delays. People forget details, chase missing information, or re-enter the same data into multiple places.
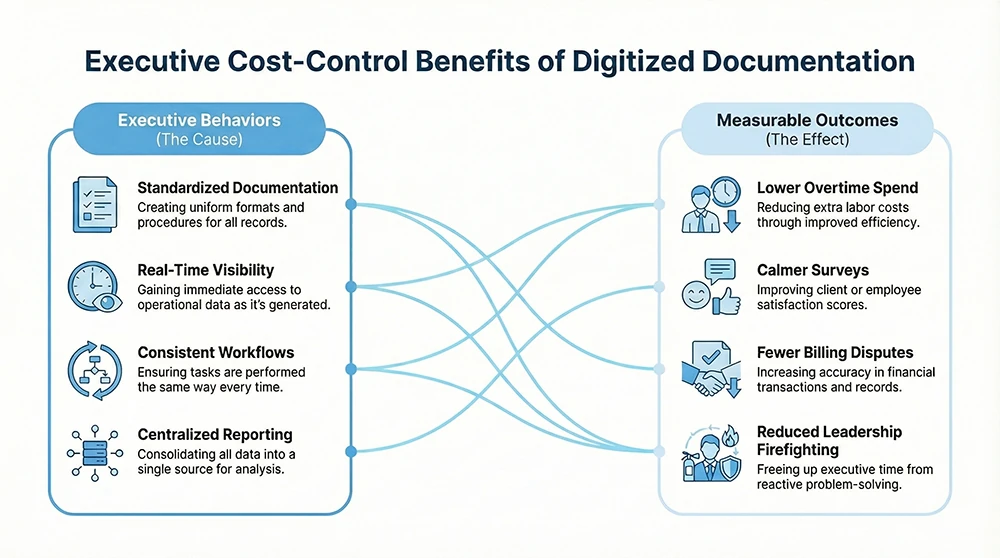
Structured documentation, task prompts, and consistent workflows reduce guesswork. Over time, you see fewer end-of-shift backlogs because the work gets done in smaller pieces throughout the day. The financial impact shows up as steadier staffing, fewer overtime spikes, and less supervisor time spent fixing records.
2. Survey Readiness That Costs Less to Maintain
Surveys Get Expensive Before Any Fine Shows Up
Even when citations do not come with large penalties, surveys still cost you. Leaders pull records. Executive directors lose hours. Regional teams travel. You may pay for consultants, mock surveys, and corrective action follow-up. You can also lose momentum on move-ins if your team is tied up responding to issues.
Oversight and deficiency reporting for assisted living services varies by state, and federal reviews have pointed out gaps and inconsistency in monitoring (3). The practical takeaway is simple. You cannot rely on informal processes to protect you.
Digital Documentation Builds Consistency Across Buildings
Digitized documentation supports survey readiness by making records easier to complete, easier to find, and easier to show. Time-stamped entries and cleaner audit trails reduce the chance of discovering missing notes at the worst moment.
When your EHR standardizes how staff document across communities, you reduce variability. Variability is where deficiencies grow. Standard workflows help ensure that good documentation habits are not limited to one strong building or one strong manager.
3. Liability and Claims Costs That Start With the Record
When a complaint becomes a claim, your documentation becomes the story. If the story is unclear or inconsistent, you spend more time and money defending it. Smaller incidents such as falls or behavior issues can still create outsized costs if records do not line up.
Digitized documentation helps because it creates clear timestamps and consistent narratives. It reduces missing records and late entries. It also shortens leadership time spent reconstructing timelines. That saves salary cost in leadership hours and reduces disruption across the building.
4. Revenue Protection Through Better Service Capture
If services are not documented, you may not be able to justify charges. This affects private pay conversations and Medicaid waiver documentation in some states (3). The loss is not always obvious. It often appears as write-offs, disputes, or time spent proving what should already be clear.
Digitized documentation links care delivery to service tracking and resident needs. If resident acuity rises, your records show it. That makes care level discussions, staffing adjustments, and billing reviews more straightforward and less time-consuming.
5. Administrative Overhead Drops When Reporting Is Centralized
Fragmented tools force your admin team to copy information, build manual reports, and chase updates. This creates ongoing payroll drag and delays decision-making.
A centralized EHR reduces that burden. Leaders can see incidents, follow-ups, and documentation gaps in one place. At the portfolio level, this makes it easier to compare performance across communities without rebuilding reports from scratch each month.
6. Turnover Costs Go Down When Documentation Feels Doable
Documentation burden is commonly linked to frustration and burnout in healthcare settings (4). Even when wages are competitive, staff may leave if daily work feels disorganized and paperwork never seems finished.
Better documentation workflows do not solve every staffing issue, but they remove friction. When charting is easier and expectations are clear, staff are less likely to stay late or feel constantly behind. Over time, that supports retention and lowers recruitment and training costs.
7. Cybersecurity and Data Loss: Avoiding the Big, Bad Day
Healthcare breaches are among the most expensive across industries. The IBM Cost of a Data Breach Report 2024 reported an average healthcare breach cost of $9.77 million (5). Even smaller incidents carry legal, operational, and reputational costs.
HIPAA’s Security Rule sets expectations for how electronic protected health information should be safeguarded (6). A HIPAA-aligned EHR supports access controls, audit trails, and secure backups that are difficult to maintain with paper records and shared drives (6) (7). The cost savings come from avoiding downtime, legal exposure, and crisis response.
8. Scaling Without Scaling Chaos
Growth magnifies weak processes. Paper-heavy documentation increases training burden, admin staffing needs, and compliance risk as you add communities.
Digitized documentation supports standardization. One way to chart, one way to report, and one set of expectations makes onboarding easier and audits faster. Even without active expansion, standardization helps you manage rising acuity and regulatory attention without adding overhead.
Conclusion: A Practical Way to Lower Cost Without Cutting Care
Digitizing documentation and reporting delivers savings where you feel them most. You see fewer overtime spikes, calmer surveys, faster incident follow-up, and less manual reporting work. Over a multi-community portfolio, small daily gains add up to meaningful financial impact.
If you are evaluating your current assisted living EHR or considering a change, the key question is practical. Where does documentation cost you the most today, and how quickly can better workflows reduce that cost across every building.
References
- Yen, P.Y., et al. “Nurses’ Time Allocation and Multitasking of Nursing Activities.” Journal of Nursing Scholarship (2018).
- Bakhoum, N., et al. “A Time and Motion Analysis of Nursing Workload.” Healthcare (2021).
- U.S. Government Accountability Office. “Medicaid Assisted Living Services: Improved Federal Oversight.” GAO-18-179 (2018).
- U.S. Department of Health and Human Services. HIPAA Security Rule Summary (2024).
- IBM Security. Cost of a Data Breach Report 2024.
- HHS Office for Civil Rights. HIPAA Security Rule Guidance.
- HHS OCR. HIPAA Security Series: Technical Safeguards.
Disclaimer:
This article provides general information for educational purposes and does not constitute legal, regulatory, financial, or compliance advice. Assisted living and memory care regulations vary widely by state and may change without notice. Requirements related to HIPAA, cybersecurity, documentation, and electronic health records depend on your organization’s structure, payer relationships, billing methods, and operational practices.
You should consult qualified legal counsel, regulatory specialists, or state licensing authorities to determine the specific obligations that apply to your communities and to verify how the guidance in this article relates to your organization’s compliance responsibilities.






.jpeg)