Regulatory Pressure On Your Documentation Is Growing

You feel it every survey cycle. Expectations around documentation keep rising, even though assisted living and memory care are regulated at the state level, not by a single federal playbook. Many states now borrow language and expectations from HIPAA, HITECH, CMS long term care guidance, and NIST security frameworks when they look at how you store and protect resident information (1)(2).
That means your records are judged not only on what they say, but on how they are created, stored, and changed over time. Surveyors, attorneys, and insurers want to see that your documentation is complete, timely, authenticated, and traceable to specific staff members. They also want to see that you can show when something was documented and whether it was changed later.
For a senior living operator with 40 or more communities, small documentation gaps do not stay small. A pattern of late entries, missing signatures, or unclear authorship across several buildings can quickly turn into regulatory risk, financial exposure, and brand damage. When your EHR captures detailed audit trails and uses digital signatures correctly, you give yourself a way to show, with evidence, how care was documented and by whom (3)(4).
What EHR Audit Trails Actually Do For You
Think about your EHR as a living record of everything that happens around resident care. An audit trail is the behind the scenes log that records every important action in that system. It tracks who logged in, who opened a chart, who created a note, what was changed, and when each step happened (3)(4).
Without an audit trail, a progress note or incident report is just a statement on the screen or on paper. With an audit trail, you can show when the note was started, how long it sat in draft, whether it was edited after an incident, and whether any parts were removed. This turns regular documentation into evidence that can be verified.
In practice, this helps you in several ways.
You can show documentation integrity. If a family member or surveyor questions whether a note was written after the fact, you can pull an audit report that shows the original entry time, any later edits, and who made them (5). This matters during investigations into falls, medication errors, elopements, and changes in condition.
You can support your cybersecurity story. The HIPAA Security Rule expects covered entities to have audit controls in place that record access and activity in electronic systems (6). NIST guidance also highlights logging and monitoring as key protections for confidentiality and integrity of data (7). Even if your communities are not always treated as full HIPAA covered entities, aligning your EHR with these expectations shows that you take security and integrity seriously.
You can spot patterns across communities. When your audit trails are easy to review, you and your regional teams can see where notes are consistently entered late, where edits happen hours after events, or where certain user roles are associated with repeated documentation problems. That information helps you target training, adjust workflows, and reduce your overall risk profile.
How Digital Signatures Raise Accountability
If audit trails tell you what happened in the record, digital signatures tell you who takes responsibility for that documentation. A digital signature ties a specific user account, at a specific time, to a specific entry.
Most state regulations require clinical and service documentation to be authenticated in some way, especially for assessments, service plans, and medication administration records (8). Handwritten signatures on paper can be hard to read, easy to copy, and easy to separate from the actual documentation page. A digital signature within your EHR is clearer and more secure.
A good digital signature system confirms the identity of the staff member, records the exact time of signing, and locks the entry so it cannot be changed without leaving a trace. This supports the legal concept of non repudiation, which means the signer cannot realistically deny that they signed the record (9).

For you, this has a very practical impact.
In medication administration, you can see who signed off on each dose for each resident and at what time.
In care plans, you can see which nurse or leader approved the plan and when.
In policy driven workflows, such as incident reviews or change in condition escalations, you can see who completed each step.
When questions come up about who knew what and when, your digital signatures give you clear, time stamped answers.
How Audit Trails And Digital Signatures Work Together
Audit trails and digital signatures are strongest when they work side by side. As an executive, you want a complete picture of each important event in your communities. That picture should include what was documented, who documented it, when it was recorded, and whether it was changed later.
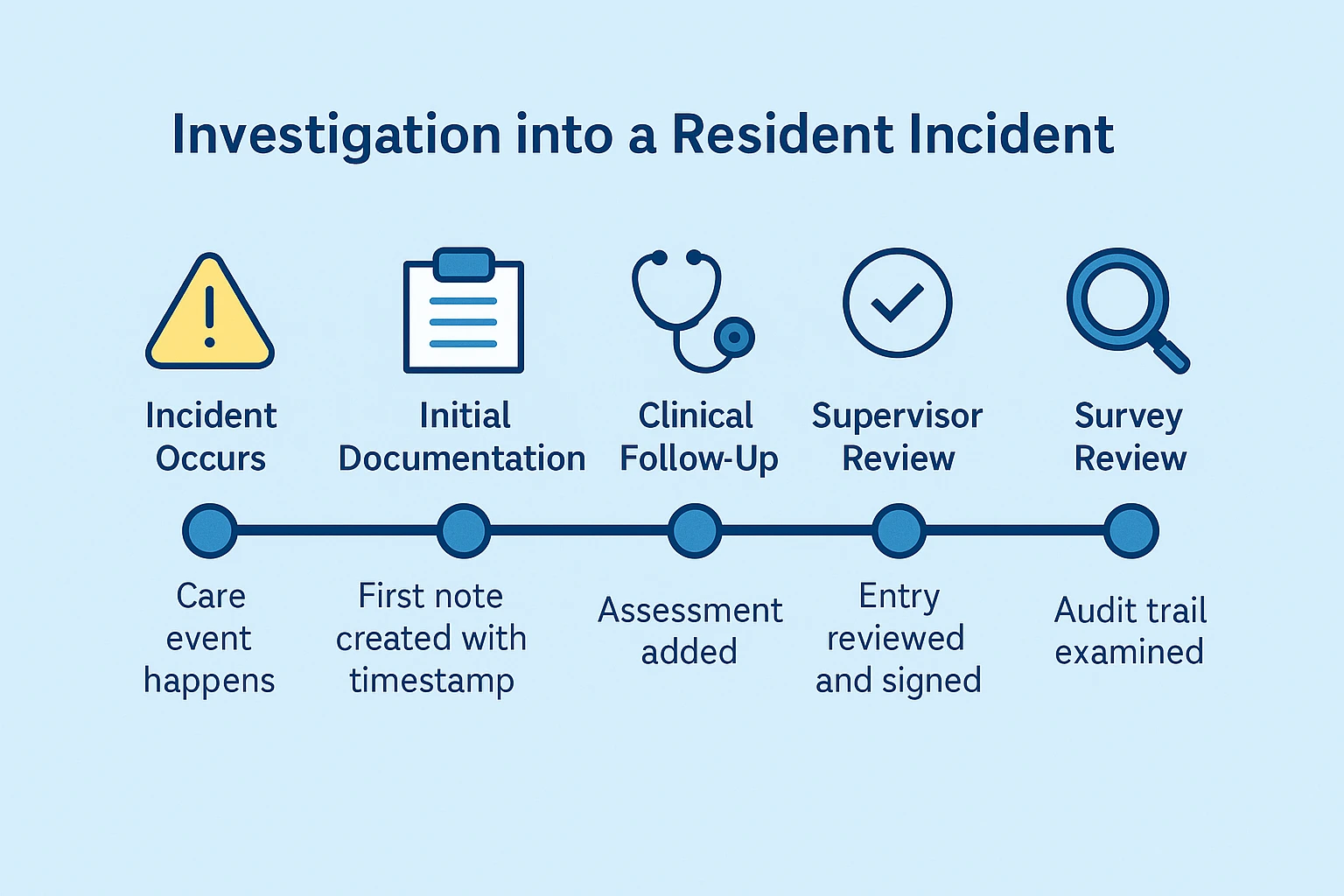
With both features active in your EHR, a typical sequence around a resident event might look like this.
A caregiver documents a fall in the resident’s record. The audit trail records the creation time and the user account. A nurse later adds details about vital signs and assessment, then signs the note with a digital signature. The audit trail logs those edits and the final sign off. If a leader or surveyor reviews the event days later, their access is recorded too.

Now imagine that same event without these controls. A note exists, but you cannot easily prove when it was created or who really wrote it. If someone suggests that staff changed the story after talking to a family or regional leader, you have no way to show otherwise.
When you have both strong audit trails and digital signatures, you gain traceability and accountability at the same time. That is what regulators, attorneys, and insurers expect when they evaluate the quality of your documentation (5)(9).
How This Plays Out In Real Incidents
To see how this protects you, it helps to walk through a few common scenarios.
In a fall investigation, surveyors and families often focus on response time, assessments, and follow up. With a detailed audit trail, you can show when the fall note was started, when vital signs were recorded, and when the nurse completed the assessment. Digital signatures show exactly who signed each piece of documentation. This combination helps you prove that staff responded and documented in line with your policies.
In an elopement or missing resident event, your logs can show when safety rounds were documented and by which staff. If a check was late or missed, that pattern appears in the audit reports. While that may create difficult conversations, it also gives you a truthful view of what happened and a clear basis for corrective action.
In medication error investigations, digital signatures tied to your electronic MARs show which staff member acknowledged and recorded each medication event. Audit trails then confirm that entries were not quietly edited after the error was discovered. This supports both honest root cause analysis and your defensibility when external parties review the case.
In changes of condition, surveyors often look closely at timelines. They want to know when first symptoms were documented, when nurses were notified, when physicians were contacted, and when families were updated. When your EHR shows a clear sequence of signed entries, backed by an audit trail, you can walk reviewers through that timeline with confidence (5).
Operational Benefits For Multi Community Operators
Defensibility creates operational ripple effects. Communities that use authenticated documentation reduce errors, improve accountability, and operate with greater clarity. Staff adapt quickly to environments where actions are visible and attributable. Training becomes data driven. Risk becomes measurable instead of speculative.
From a legal standpoint, organizations with strong digital documentation close cases faster, spend less on discovery, and experience fewer compliance related disputes. Insurers favor organizations that can prove care delivery with system native audit histories.
Families, too, benefit. You can explain in straightforward language that your system shows who did what and when, and that it records changes automatically. That level of clarity builds confidence in your care model over time.
Signs That Expectations Are Tightening
Across the country, several states are exploring or updating standards that touch on electronic documentation, record integrity, and authentication for assisted living and memory care (10). At the same time, federal agencies and national organizations continue publishing guidance about secure health information practices, audit controls, and electronic signatures (1)(3)(6)(7)(9).
Taken together, these trends point in one direction. Regulators, attorneys, and insurers expect providers to maintain records that are accurate, secure, and traceable. They also expect leaders to show how their systems prevent or detect tampering.
If your EHR already includes strong audit trails and digital signatures, you are positioned to meet these expectations with less friction. If those features are weak or inconsistently used, this is the right time to review your configuration, policies, and training approach.
Conclusion
You manage a complex organization with teams working around the clock across dozens of communities. When something goes wrong, your documentation is often the first thing people ask to see.
Strong audit trails and reliable digital signatures allow you to respond with records that are time stamped, user specific, and complete. They help you show how care was delivered, how decisions were made, and how information moved through your organization.
Clear documentation does not eliminate risk, but it does reduce uncertainty. In a regulatory environment that rewards proof and traceability, organizations that treat audit trails and digital signatures as core controls will be better prepared to protect residents, staff, and operations as expectations continue to rise (2)(4)(5)(8)(10).
References
- U.S. Department of Health and Human Services, HIPAA Privacy Rule guidance.
- Centers for Medicare and Medicaid Services, long term care regulatory and survey guidance.
- U.S. Department of Health and Human Services, Office for Civil Rights, audit control requirements.
- Health Information Technology for Economic and Clinical Health Act provisions for electronic records.
- U.S. Department of Justice, healthcare documentation and fraud prevention guidance.
- HIPAA Security Rule, technical safeguards for electronic health information.
- National Institute of Standards and Technology, Special Publication 800-53.
- State assisted living and residential care statutes and regulations, documentation requirements.
- Electronic Signatures in Global and National Commerce Act.
- Emerging state policy initiatives on electronic documentation and record integrity.
Disclaimer:
This article provides general information for educational purposes and does not constitute legal, regulatory, financial, or compliance advice. Assisted living and memory care regulations vary widely by state and may change without notice. Requirements related to HIPAA, cybersecurity, documentation, and electronic health records depend on your organization’s structure, payer relationships, billing methods, and operational practices.
You should consult qualified legal counsel, regulatory specialists, or state licensing authorities to determine the specific obligations that apply to your communities and to verify how the guidance in this article relates to your organization’s compliance responsibilities.