The New Regulatory Reality You Are Working In
Regulation around assisted living and memory care is getting stricter and more detailed. Many states are raising expectations for assessments, service plans, staff documentation, incident reporting, and resident protections in licensed communities. (6) Federal agencies also influence you through HIPAA privacy and security rules, civil rights guidance, and health IT regulations whenever you handle electronic protected health information, or ePHI. (1)(7)
If you operate 40 or more communities, this pressure does not hit only one building at a time. It shapes how you design your systems, how you train staff, and how you manage risk at a corporate level. Your EHR is now central to that work. It sits at the heart of privacy compliance, cyber protection, survey response, and wellness reporting.
Some assisted living communities are clearly HIPAA covered entities because of the way they bill and the payers they work with. Others may become covered entities as service lines and billing practices change. In either case, the HIPAA Security Rule sets standards for how you protect ePHI in electronic systems, including your EHR. (1)
When you look at your EHR, you are not only asking how it supports caregivers. You are also asking how it helps you prove that care is safe, consistent, and well governed across your entire portfolio.
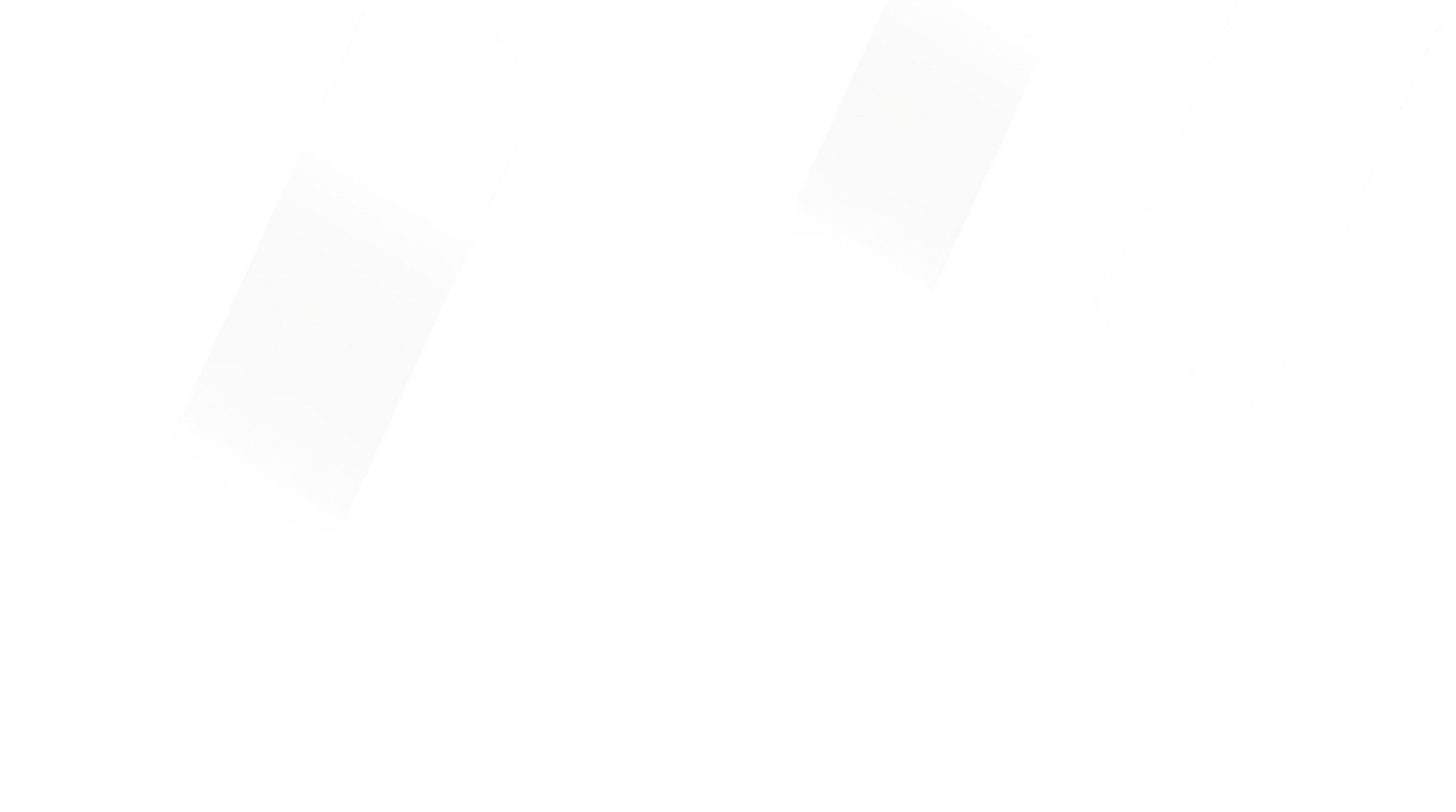
Mapping Regulations to Clear EHR Requirements
You can make this work easier by turning a complex mix of rules into a simple map that your teams can follow.
First, you identify the main layers of regulation that apply to your organization. HIPAA is one of those layers. It requires a risk analysis, access controls, audit logs, and contingency plans to protect ePHI. (1) The HIPAA Right of Access also gives residents, and the people they designate, the right to see and receive copies of their health information within defined time frames and at reasonable cost. (2)
Another layer comes from information blocking rules under the 21st Century Cures Act. These rules focus on electronic health information, often called EHI. They define practices that interfere with access, exchange, or use of EHI and make many of those practices unacceptable unless a specific exception applies. (3)(4)
A third layer involves certified health IT. Assisted living providers do not have to use ONC certified technology. Still, when an EHR is designed in line with ONC certification criteria, it usually supports better interoperability and clearer expectations for security and data handling. (5)
On top of these federal expectations, each state sets its own rules for assisted living and memory care. These rules may define what must be in assessments, how often service plans are updated, how incidents are reported, and how medications are documented. (6) Civil rights guidance adds expectations around equal treatment, proper use of assessment tools, and support for people with disabilities in long term care. (7)
After you have this stacked view, you can build a simple compliance matrix. On one side, list the rules and guidance that apply. On the other side, list the EHR features, workflows, policies, and training that respond to each one. That matrix can guide both your EHR configuration and your survey story.
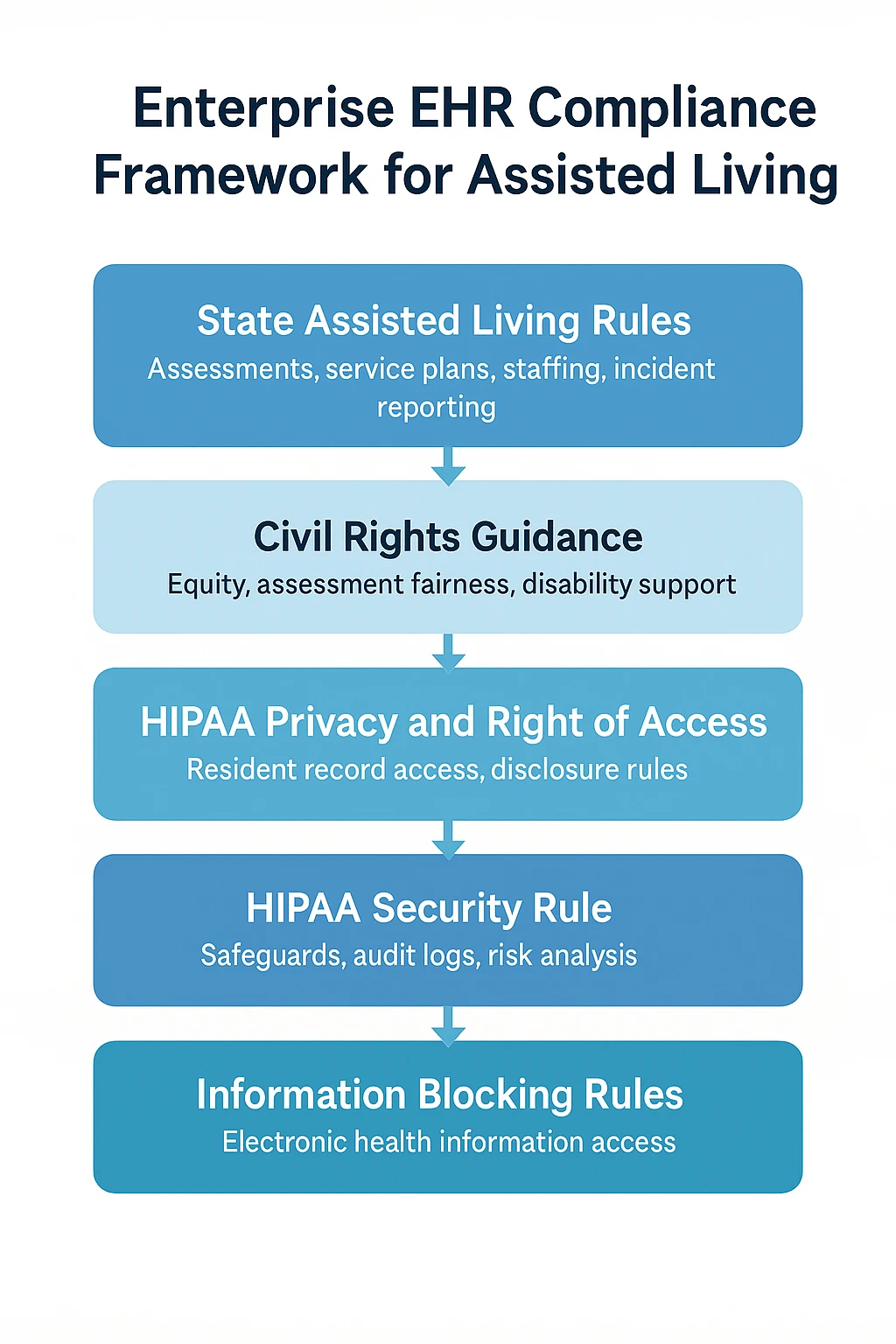
Strengthening Security, Privacy, and Cyber Resilience
Security and privacy are not optional features for your EHR. They are legal and ethical requirements. The HIPAA Security Rule talks about three kinds of safeguards: administrative, physical, and technical. Together, they control who can access data, how devices and facilities are protected, and how the technology itself resists misuse or attack. (1)(8)
For you, this usually means that your EHR should support strong, role based access, detailed audit logs, and encryption for data at rest and in transit. It should also support secure remote access for leaders, wellness teams, and clinical partners, without creating easy entry points for attackers. (8)(9)
Federal guidance and industry checklists now encourage or expect multi factor authentication, more formal security risk assessments, and clear incident response plans. (8)(9) Recent compliance resources also highlight the need for current inventories of systems and data flows, so you can show where resident information moves across your communities and vendors. (8)(9)
When you select or review an EHR, you and your IT partners can ask for evidence of these safeguards. You can also ask vendors how they handle security incidents, how often they test controls, and how they support you in meeting HIPAA expectations.
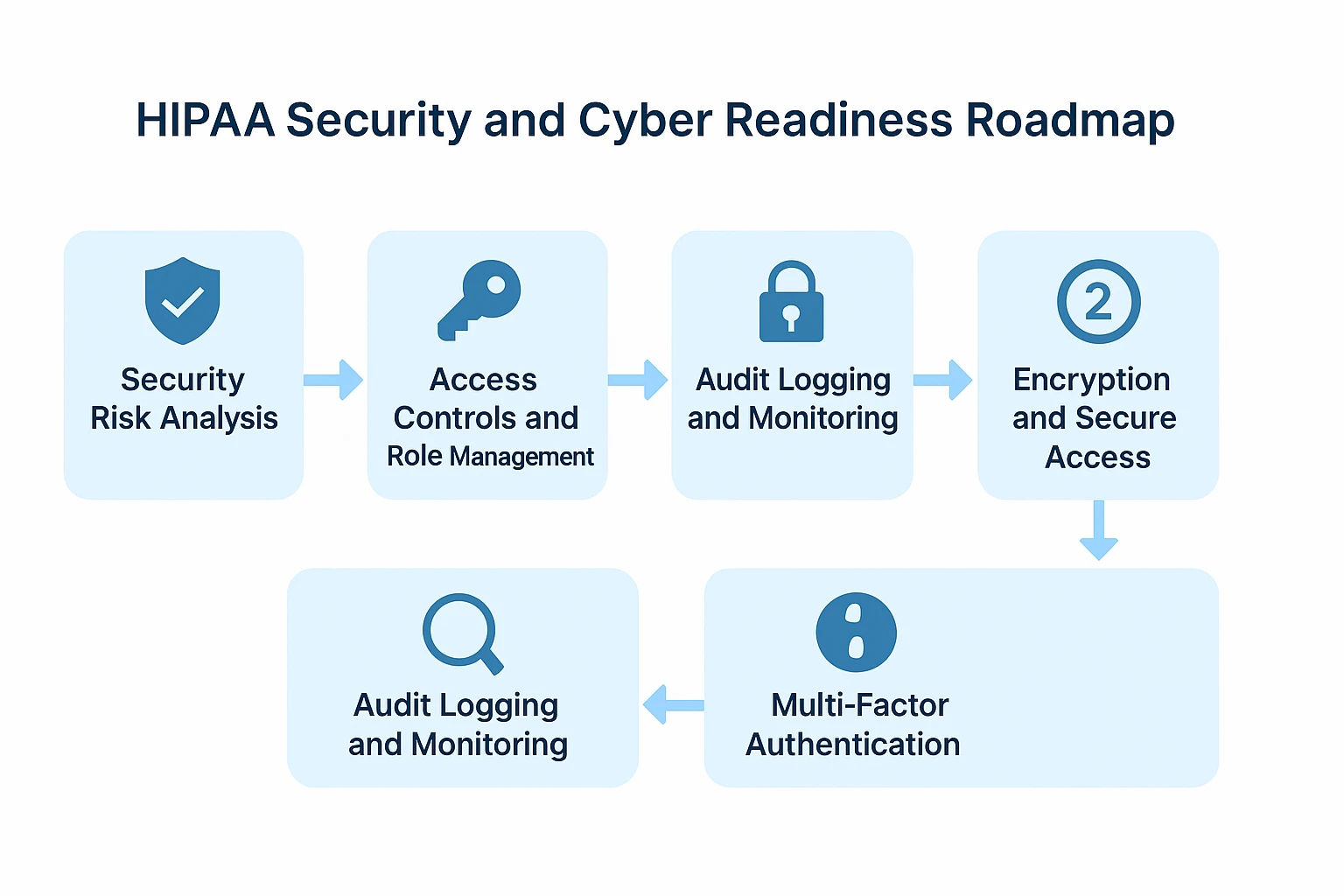
Documentation That Supports Surveys and Risk Management
Surveyors are less interested in what you say your processes are and more interested in what shows up in the record. State regulatory reviews show growing focus on the quality and completeness of documentation in assisted living settings. (6)
For your communities, this means that assessments should match state requirements, care plans should clearly connect back to assessments, and daily documentation should show that planned services are being delivered. Incident records for falls, elopements, behavioral changes, or medication errors should provide enough detail to explain what happened, how staff responded, and what follow up occurred.
Many senior living EHR platforms now offer state aligned templates, service plan tools, incident forms, and reminders that support this kind of survey readiness. (10) Those features only help when they are configured correctly and used consistently. Your role is to encourage standard use across locations and make sure leaders review data for patterns and gaps.
Good documentation is also one of your best tools for risk management and wellness improvement. When caregivers record changes in weight, mobility, behavior, and engagement, you can see patterns across communities and across time. These patterns support more targeted wellness programs, staffing decisions, and environment changes.
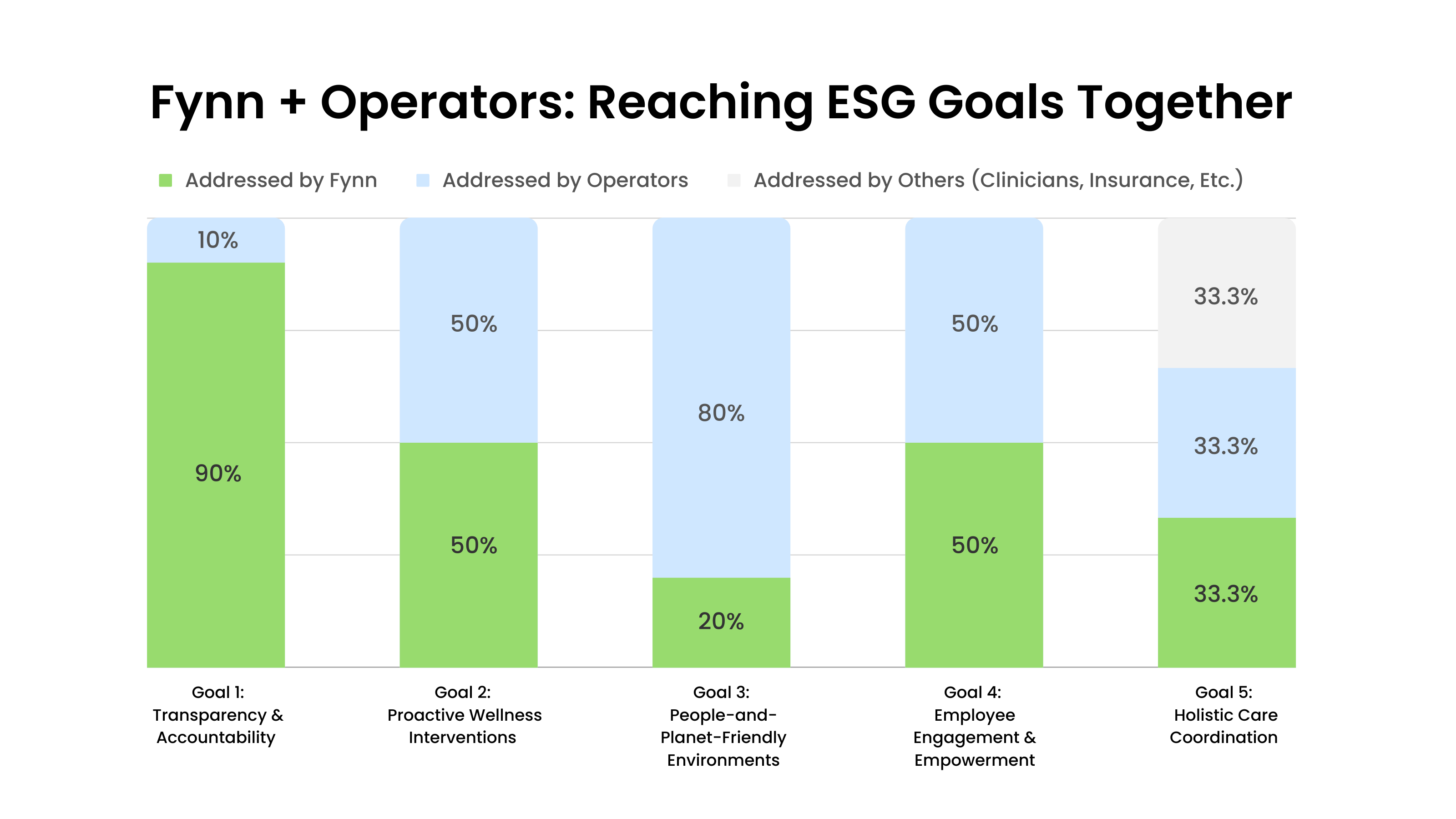
At this stage, choosing technology that is designed around senior living workflows can help a great deal. For example, using the dedicated platform from Fynn, which is built for assisted living and memory care, can improve documentation workflows and real time visibility for leaders and wellness teams. That kind of visibility supports both regulatory performance and resident quality of life.
Supporting Interoperability and Information Access
Your communities do not work in isolation. Residents move between hospitals, rehab, hospice, primary care, and your buildings. Information blocking rules recognize this movement and aim to reduce unnecessary barriers when electronic health information needs to flow. (3)(4)
For you, this means your policies and your EHR setup should avoid avoidable delays, unreasonable fees, or confusing processes when other providers, residents, or families request access to appropriate information. You still protect privacy and follow the rules, but you do not hide behind the system or contracts when there is a lawful right to share data. (3)(4)
The HIPAA Right of Access is a key part of this story. Residents and their designated representatives must be able to get information in a timely way, in a usable format, at a reasonable cost. (2) That can include electronic copies, view access through a portal, or other agreed upon methods.
An EHR that supports simple record requests, family portals, and clear export options makes this much easier. When you add training for front line teams on how to respond to access requests, you reduce friction, complaints, and risk.
Governance, Training, and Change Management
Even a strong EHR will not solve compliance problems if governance and training are weak. Regulations change. Cyber threats change. Your service mix and payer mix can change too. A one time implementation is not enough.
Many operators find it useful to create an EHR governance group that brings together wellness leaders, nursing leaders, operations, IT, compliance, and risk. That group can review new laws and guidance, decide what EHR changes are needed, and oversee how those changes are rolled out.
Training is the other half of this work. Caregivers, nurses, and managers need simple, concrete examples of what good documentation looks like in your system. They also need reminders of why documentation matters for resident safety, survey results, and your brand.
You can use de identified real cases from your own communities to show both strong and weak documentation. Over time, you and your leaders can build a culture in which complete, accurate, and timely EHR documentation is seen as part of good care, not just extra work.

Evaluating EHR Vendors for Regulatory Readiness
When you look at an EHR vendor, you are not only buying features. You are choosing a long term partner in risk and compliance.
From a security view, you can ask vendors to explain how they meet HIPAA Security Rule expectations, such as encryption, access controls, audit logging, and multi factor authentication. (1)(8)(9) You can also ask how they notify you about security incidents and how they support you during a breach investigation.
From an interoperability view, you can ask whether the system or its components align with ONC Health IT Certification criteria, since those criteria reflect expectations around data formats, exchange, and safety. (5) From a regulatory view, you can check how easily the system handles different state requirements for assessments, care plans, and reports across your footprint. (6)(10)
Contract terms also matter. You want clarity about data ownership, export rights, support levels, uptime commitments, and business associate agreement details when HIPAA applies. These items become very important when you add new communities, close locations, or change service lines.
Building an Enterprise EHR Roadmap for Compliance and Wellness
Your goal is not just to have an EHR in each building. Your goal is to have an enterprise level EHR program that supports regulation, risk management, and wellness across all assisted living and memory care communities.
A practical roadmap often starts with a baseline assessment. In that step, you compare your current EHR setup against HIPAA privacy and security expectations, state regulatory requirements, and information blocking rules. (1)(3)(6) You look at which features you are using, which policies exist only on paper, and where documentation falls short.
Next, you and your IT and compliance partners can complete a focused risk and gap analysis. This work may cover access control, device security, encryption, incident response, vendor oversight, and staff training. (8)(9) The result should be a short list of the most important actions that will reduce risk and support regulations.
You can then move into standardization. Core workflows, such as assessments, service planning, incident reporting, and medication documentation, should follow consistent patterns across communities, even if you allow local variations for state rules. (6)(10)
As you strengthen workflows, you can also build wellness and outcomes metrics into your reporting. Falls, activity engagement, behavioral patterns in memory care, and weight trends can all feed into dashboards that you review with local and corporate leaders. (10) These dashboards help you connect regulatory expectations to real resident outcomes.
Finally, your roadmap should include ongoing governance, training, and yearly reviews. That way, your EHR program stays aligned with new rules, new threats, and new service models.
When you approach EHR planning in this way, the system becomes more than a place where staff chart tasks. It becomes a shared tool that supports regulatory compliance, resident wellness, and consistent performance across your organization.

References
- U.S. Department of Health and Human Services. Summary of the HIPAA Security Rule.
- HHS Office for Civil Rights. Individuals’ Right under HIPAA to Access their Health Information.
- Office of the National Coordinator for Health IT. Information Blocking Overview.
- American Medical Association. What Is Information Blocking? Part 1.
- ONC. About the ONC Health IT Certification Program.
- National Center for Assisted Living. Assisted Living State Regulatory Review.
- HHS Office for Civil Rights. Civil Rights Guidance for Long Term Care Facilities.
- McGuireWoods. HIPAA Security Rule Compliance for Senior Living and Long Term Care Providers.
- HIPAAJournal. HIPAA Security Rule Safeguards and 2025 Compliance Checklist.
- ECP. What Is EHR in Assisted Living and Why It Matters.
Disclaimer:
This article provides general information for educational purposes and does not constitute legal, regulatory, financial, or compliance advice. Assisted living and memory care regulations vary widely by state and may change without notice. Requirements related to HIPAA, cybersecurity, documentation, and electronic health records depend on your organization’s structure, payer relationships, billing methods, and operational practices.
You should consult qualified legal counsel, regulatory specialists, or state licensing authorities to determine the specific obligations that apply to your communities and to verify how the guidance in this article relates to your organization’s compliance responsibilities.







.jpeg)