You have likely experienced moments when one incident created days of follow-up work. A fall or medication error happens, the family is upset, and you spend time recreating timelines from scattered notes. These situations become even harder when documentation is incomplete. Regulators and attorneys often begin their review by asking for incident records, and the quality of those records shapes how the rest of the process unfolds.
Your communities operate under a patchwork of rules. State licensing boards require specific types of reporting, and insurers expect consistent documentation. Federal regulations also come into play. Any system that stores resident health information must follow the HIPAA Security Rule, which includes administrative, physical, and technical safeguards for electronic health information (1). These expectations create a real need for clear and accurate records.
Falls illustrate the challenge well. They are the leading cause of injury for older adults, and millions of people age 65 and older report a fall each year (2). When a fall takes place in one of your buildings, the questions arrive quickly. Families want reassurance. Inspectors want proof that your staff responded appropriately. If your documentation is late or missing details, you may have a harder time defending your community’s actions.
Risk and insurance experts consistently point out that accurate and timely documentation helps protect organizations during disputes (3). Their guidance aligns with what you probably see in your own operations. When documentation is structured and consistent, your teams are better prepared to manage difficult situations. When it is not, small gaps can turn into large problems.
This is where an assisted living EHR supports you. When incident tracking is part of the system your caregivers already use, documentation becomes a routine part of care. Instead of filling out paper forms or trying to remember details at the end of a shift, staff enter information directly into the EHR while the event is fresh in their minds. Each report includes the time, date, location, and people involved.
Structured formats help reduce errors. Studies have shown that documentation compliance improves when staff follow clear templates and receive regular feedback, sometimes increasing accuracy to more than seventy percent (4). With an EHR, these templates are built into the workflow, which reduces guesswork. Your quality team can also review reports more easily and identify locations that may need additional support.

You gain even more value when incident records connect to the rest of the resident’s chart. A behavior event links to the care plan. A medication issue connects to the resident’s orders. After a fall, the assessment can be updated on the spot. The feature overview for the Fynn EHR, which outlines real-time documentation and resident risk tools, describes how these elements come together in practice. This kind of integration helps your staff understand each resident’s full picture.
Regulators and attorneys often focus on the timeline of an incident. They want to know who found the resident, who the team contacted, and how quickly actions were taken. An EHR record with time-stamped entries gives you that timeline. It shows the sequence of events clearly, which helps you demonstrate that your team followed proper procedures.
Quality improvement also benefits from this approach. CMS describes QAPI as a data-driven method for understanding adverse events and improving systems over time (5). Even though not all senior living communities fall under CMS requirements, the same principles apply. When your incident data is consistent, your leadership team can identify patterns that signal a need for change. This could be a hallway with frequent falls or a resident whose behavior incidents are increasing.
Rolling out EHR-based incident tracking requires leadership support. When you define what counts as an incident and make sure the expectations are the same across all buildings, your teams gain clarity. This reduces confusion and builds confidence. When caregivers have access to devices that allow point-of-care documentation, the process becomes quicker and easier.
Training also plays a central role. You can help teams understand that strong documentation protects residents, protects them, and protects the organization. Regular reviews and coaching sessions create a cycle of learning. Research on documentation shows that feedback helps staff improve their accuracy and consistency (4). Small changes, repeated over time, make a measurable difference.
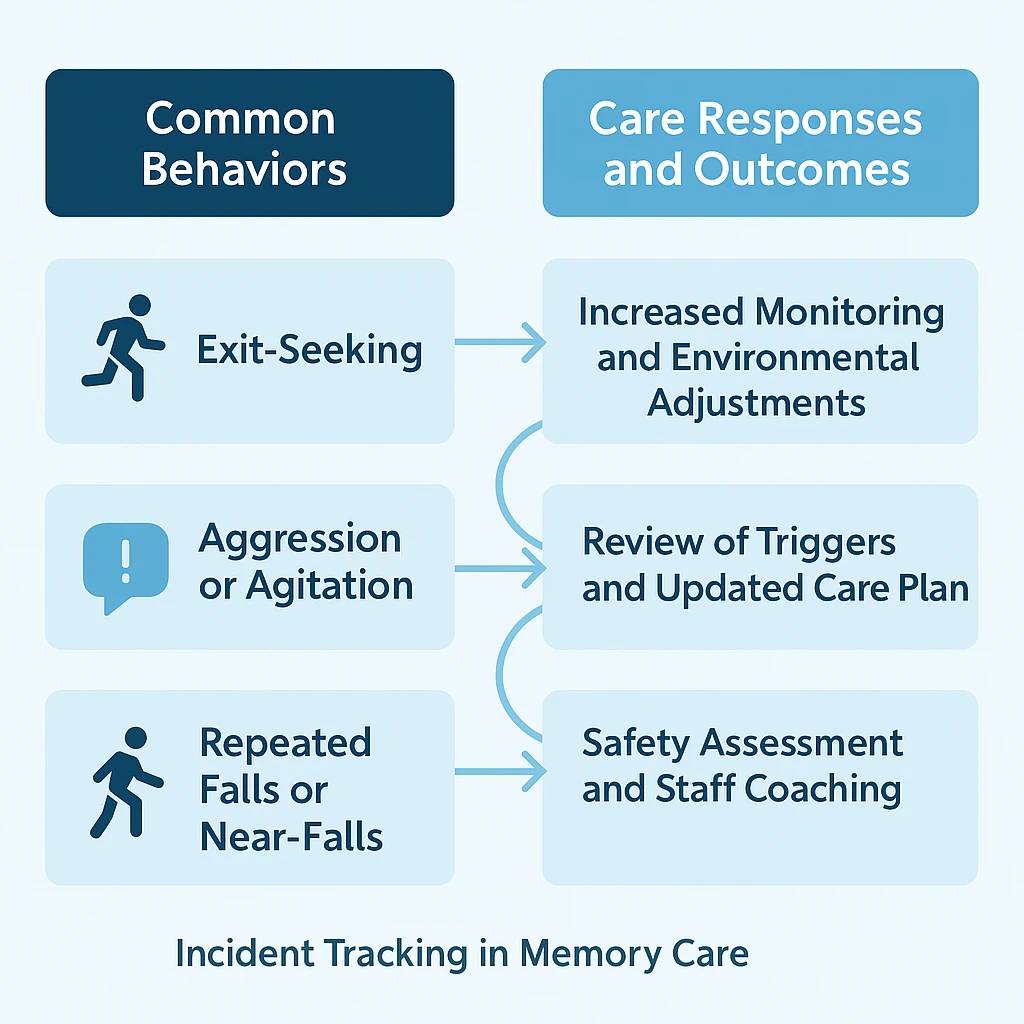
Memory care environments add another layer of complexity. Residents may wander, misinterpret situations, or react strongly to changes around them. Families may have high expectations and emotional involvement. In these situations, incident tracking helps create a clear record of behavior patterns, triggers, and staff interventions. This record is valuable during care-plan updates and during discussions with family members who want a better understanding of what their loved one is experiencing.
When incident tracking is consistent, you can also identify residents or locations that present higher risk. If a particular wing has repeated issues during certain hours, you can adjust staffing or environmental design. When a resident shows increased agitation or exit-seeking, you can review interventions more quickly. This type of pattern recognition can prevent serious events.
A well-organized incident tracking program helps your bottom line as well. Better documentation can reduce claim costs and improve your standing with insurers. Leaders spend less time searching for missing information and more time supporting residents and staff. When you can show strong documentation practices to lenders, partners, or potential buyers, you strengthen your organization’s position.

You cannot prevent every incident, but you can control how your organization responds. An assisted living EHR with reliable incident tracking gives you a clearer record of what happened, what actions were taken, and how your team addressed the issue over time. It provides structure and consistency across all your communities. Most importantly, it supports your goal of keeping residents safe and giving staff the tools they need to work confidently.
References
- U.S. Department of Health and Human Services. “The Security Rule.” HIPAA for Professionals.
- Centers for Disease Control and Prevention; National Council on Aging. Older Adult Falls Data and Falls Prevention Factsheets, United States.
- Gallagher. Reports on staff documentation in assisted living communities, including legal defensibility considerations.
- Bunting J, de Klerk M. “Strategies to Improve Compliance with Clinical Nursing Documentation Guidelines in the Acute Hospital Setting.” 2022.
- Centers for Medicare and Medicaid Services. “Quality Assurance and Performance Improvement (QAPI): Description, Background, and Adverse Events Resources.”
Disclaimer:
This article provides general information for educational purposes and does not constitute legal, regulatory, financial, or compliance advice. Assisted living and memory care regulations vary widely by state and may change without notice. Requirements related to HIPAA, cybersecurity, documentation, and electronic health records depend on your organization’s structure, payer relationships, billing methods, and operational practices.
You should consult qualified legal counsel, regulatory specialists, or state licensing authorities to determine the specific obligations that apply to your communities and to verify how the guidance in this article relates to your organization’s compliance responsibilities.






.jpeg)