The Compliance Gap You Feel Between Your Organization and Large Chains
As a COO of a small senior living operator, you live under the same regulatory expectations as much larger organizations. Federal privacy rules, state requirements for documentation, medication oversight, and resident safety do not change because you have five to ten communities instead of hundreds (1). Regulators focus on the resident, not the size of the company that owns the building.
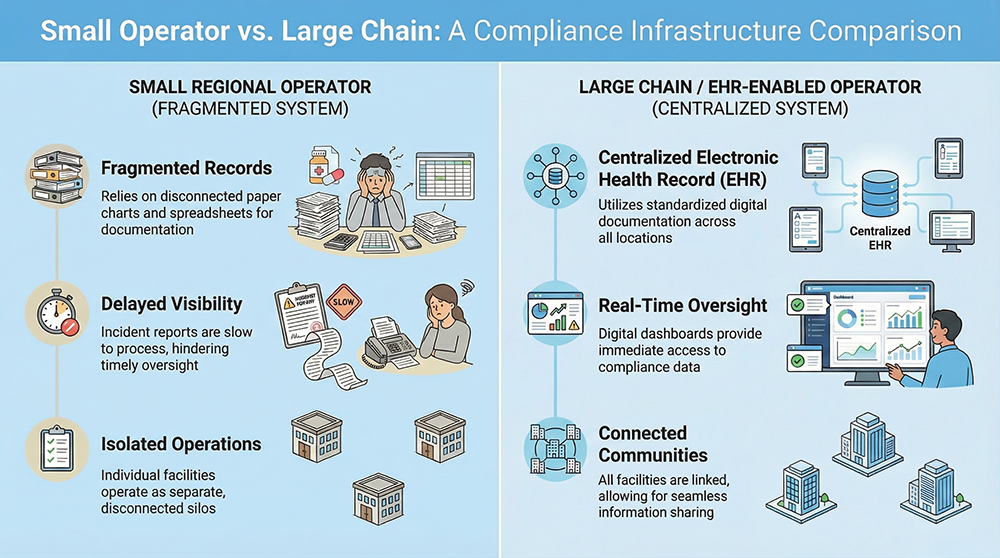
Large chains have centralized compliance departments, in-house legal support, enterprise IT teams, and standardized systems to support every survey and investigation. Your world probably looks different. Many small operators rely on local administrators and wellness directors to juggle staffing, family communication, and compliance at the same time. Documentation may sit in paper charts, static spreadsheets, or systems that do not talk to each other (2).
When records are scattered, it becomes harder for you to know what is actually happening in each building. That gap in visibility turns into a gap in risk control. Over time, this is what creates the feeling that big chains are “safer” in the eyes of regulators and insurers. In most cases, they are not more careful. They simply have better infrastructure.
What Compliance Resilience Really Means For You
Compliance resilience is your ability to stay aligned with rules and standards when something goes wrong. It shows up when you have a new executive director, when a major incident occurs on a weekend, when a surveyor arrives unannounced, or when a family attorney requests records.
In senior living and memory care, real resilience includes accurate documentation of care, clear medication records, prompt incident reporting, solid infection control practices, consistent care plans, and the ability to produce records quickly when they are requested (3). States are also looking for proof that you monitor your own performance and take action, not just that you respond when they call you (4).
If your systems are manual, you rely on everyone doing the right thing, in the right way, every day. If your systems are digital and consistent, you rely on workflows and checks that support people, especially on busy days. That is the shift you are trying to make.
How an Assisted Living EHR Levels the Playing Field
Modern assisted living and memory care EHR platforms give you access to the same kind of clinical and compliance infrastructure that large chains use. You do not need a big IT team for this. The core advantage comes from three simple ideas.
First, you move from loose, paper-heavy documentation to structured electronic records. Second, you standardize how care, medication, and incidents are documented in all communities. Third, you gain real-time access to what is happening in each building.
When those three things are in place, an EHR stops being “just software.” It turns into the backbone of how you show regulators, families, and insurers that your organization is serious about compliance.
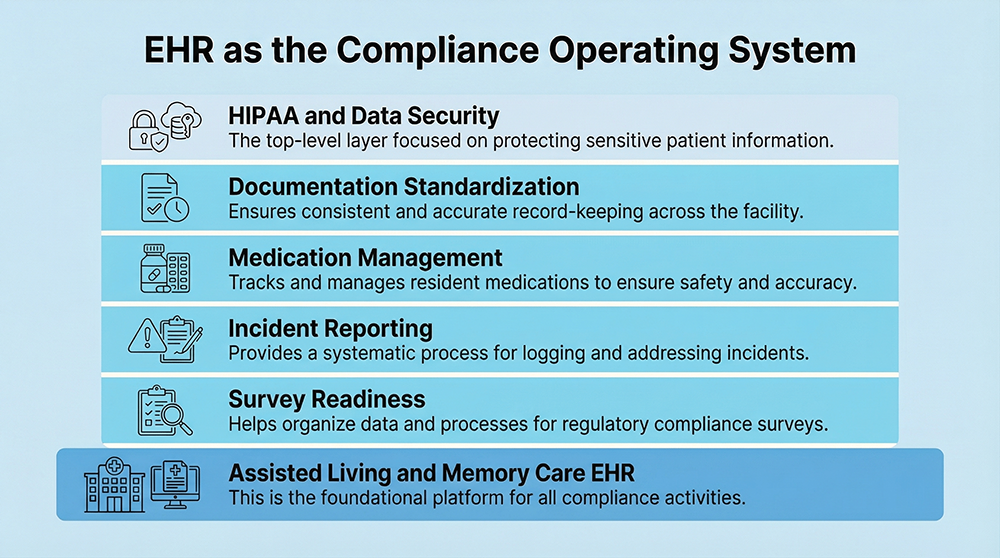
Standardizing Documentation Across Your Communities
Many small operators discover citations that relate to inconsistent documentation from building to building (5). One community has detailed care plans. Another documents only the basics. The surveyor who sees both locations in the same year will describe this as a system problem, not a single-site problem.
An EHR gives you a single structure for care plans, ADL notes, progress notes, vital signs, and other documentation. You can set required fields, use common templates, and create clear expectations for how and when staff document care. When everyone uses the same structure, it becomes much easier to prove that you follow consistent standards across your portfolio (6).
You also benefit in day-to-day operations. When a leader transfers from one community to another, they recognize the workflows and screens. This reduces the risk that local habits override your organizational standards.
Strengthening Memory Care Documentation
Memory care adds another layer of risk. Residents are more vulnerable. Behaviors can escalate quickly. Regulations and guidance around dementia care, psychotropic medication use, and safety measures are becoming more detailed and strict (7).
If you rely on handwritten behavior logs or notes tucked into paper charts, you will struggle to show clear patterns over time. After an incident, you may have to pull notes from multiple binders to explain what really happened.
With a memory-care aware EHR, your staff can document behaviors, redirections, and safety interventions in real time. You can see trends at the resident level, at the unit level, and across communities. You can also connect psychotropic medications to diagnoses and non-pharmacologic interventions, which is a growing focus area for regulators and advocacy groups (8).
This kind of record helps you support care decisions, reduces the risk of inappropriate medication use, and improves your defensibility if a complaint or lawsuit arises.
Making Medication Management Safer and More Defensible
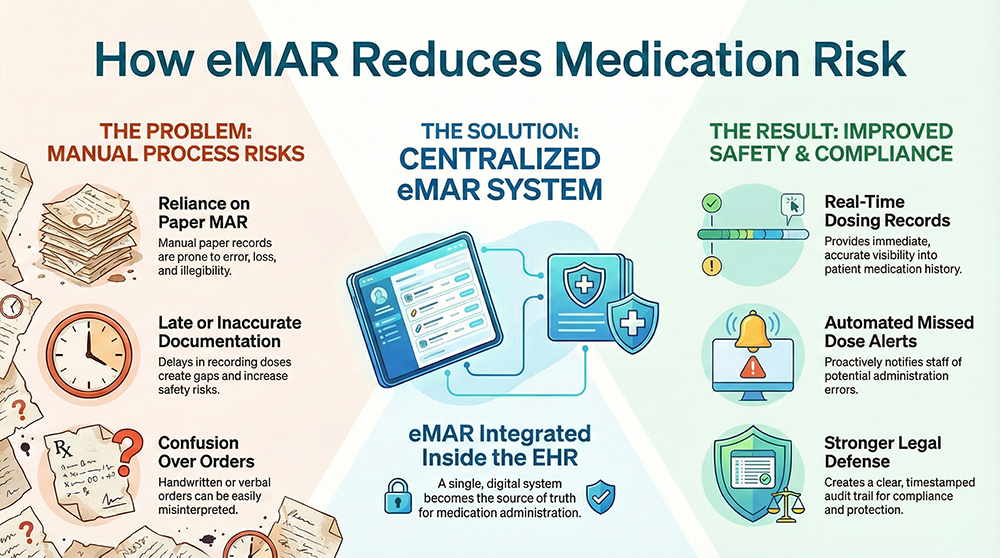
Medication errors and documentation issues remain some of the most common and serious problems in senior living and memory care settings (9). Missed doses, late administration, unclear orders, and poor records can all drive citations and lawsuits.
Paper MARs increase this risk. Staff may document at the end of the shift instead of at the time of administration. Orders can be hard to read. Changes do not always reach everyone who needs to know.
An EHR that includes an electronic medication administration record changes this pattern. Staff document as they give medications. The system can flag late or missed doses. Orders are clearer and easier to audit. Over time, you build a complete medication story for each resident, which is exactly what regulators and attorneys look for when something goes wrong (10).
For you as COO, this means fewer surprises, stronger audit data, and a clearer view of which communities need coaching or support.
Turning Incident Reporting Into Real Risk Control
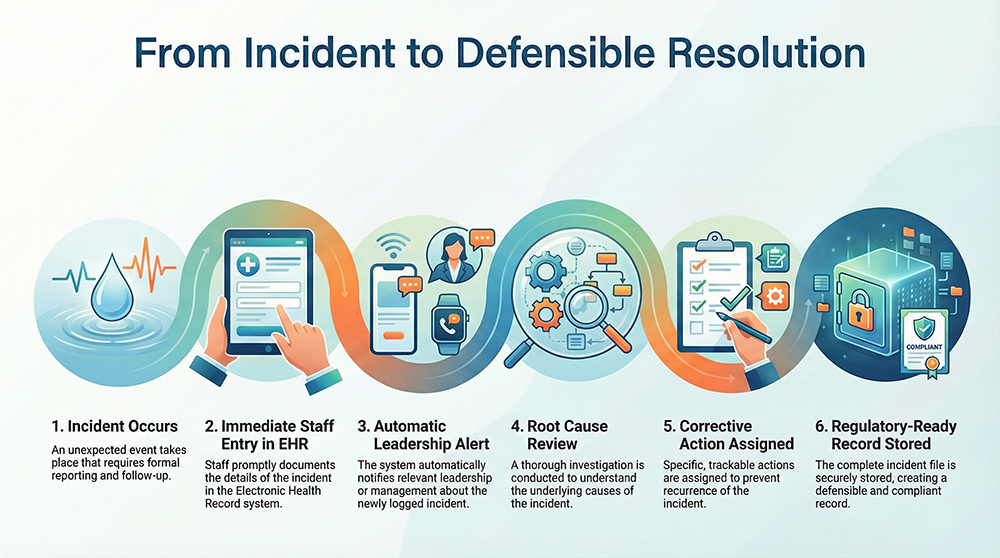
In many small organizations, incident reporting is slow and inconsistent. A fall might be documented on paper onsite, then typed into a form later, then sent to the home office some days after. By then, key details and follow-up steps may already be fuzzy.
An EHR can move incident reporting into real time. Staff enter incidents in the system soon after they occur. Leaders receive alerts. Follow-up tasks can be assigned and tracked inside the same system. You can categorize incidents, identify patterns, and show how you are learning from events instead of just logging them (11).
This approach supports both regulatory expectations and your own internal standard. You go from a “log and forget” mindset to a “log, act, and verify” cycle, which is at the heart of strong risk management.
Staying Survey Ready All the Time
With manual systems, survey readiness often feels like a scramble. You hear about an upcoming visit. Teams start pulling charts, reviewing care plans, and cleaning up documentation. This is stressful for everyone and often exposes gaps you did not know existed.
An EHR supports a “always ready” posture. Records are organized and searchable. Care histories are easy to follow. Reports can be pulled in minutes instead of days. You can audit your own documentation before a surveyor arrives and correct gaps along the way (12).
Over time, this reduces the emotional load on your teams and signals to regulators that you treat compliance as a daily practice, not a one-time performance when they walk in the door.
Protecting Data, Privacy, and Trust
Data security and privacy are no longer optional topics in senior living. Health information breaches are increasing, and many involve smaller organizations that do not have strong access controls or secure storage practices (13).
HIPAA enforcement actions do not give small organizations a free pass. Regulators have made it clear that covered entities of all sizes are expected to protect resident information using appropriate safeguards (14).
A well-designed EHR helps you meet these expectations. Role-based access limits who can see what. Logs show who viewed or changed a record. Encryption and secure hosting protect data from casual access or loss. Automatic timeouts reduce the risk of someone leaving a chart open on a shared workstation.
For residents and families, this builds trust. For you, it reduces the chance that a single lost device or file mishandling incident turns into a major regulatory event.
Giving Regional Leaders Real Visibility
One of the most important benefits of an EHR is something you feel, not just something you document. It is the shift from guessing to knowing.
With centralized reporting, you can see which communities are keeping up with documentation, where medication issues are more common, which memory care units have higher incident rates, and where staffing patterns may be stressing the system. You do not need ten different spreadsheets and phone calls to piece this together (15).
This visibility helps you focus your energy. You can put support where it is needed, reward teams that are doing well, and identify training needs early. Over time, the EHR becomes not only a clinical record, but also a leadership tool.
Using EHR Data as a Shield in Disputes
When a serious event occurs, the quality of your documentation often shapes the outcome. Attorneys and regulators look for clear, timely, and consistent records that show what your teams did, when they did it, and how they communicated with families and physicians.
EHR records typically include timestamps, user IDs, and audit trails that show how information changed over time. This kind of detail is difficult to fake and easy to explain. It carries more weight than incomplete or inconsistent paper notes (16).
For a small operator, this can be the difference between a manageable settlement and a large, organization-threatening claim. It can also influence how a regulator views your culture and systems after an adverse event.
Growing Without Losing Control of Compliance
Growth is exciting. It is also risky. Every new community adds a new set of staff, residents, and local patterns. If your systems are not prepared, compliance can start to slip just as your reputation and exposure are growing.
With an EHR in place, each new building joins a shared structure. You can roll out standard templates, training, and expectations instead of reinventing workflows from scratch at every site. Leaders moving between communities already know the system, which brings stability during change (17).
This is how you scale without losing control. You keep your culture of care while raising your consistency of practice.
[Insert Visual 5: Scaling Without Compliance Breakdown]
The Financial Case For EHR as Compliance Infrastructure
EHR conversations often focus on staffing efficiency or billing, which matter. However, the biggest financial impact for many small operators comes from avoided risk.
A single severe citation, lawsuit, or public incident can cost far more than the total subscription cost of an EHR over several years. Penalties, settlements, legal fees, insurance premium increases, and occupancy loss all add up quickly (18).
When you invest in an EHR that is designed for compliance, you are not just buying software. You are reducing the chance of high-cost events that can slow or even stop your organization’s growth.
Bringing Big Chain Discipline To a Small Operator
Your goal is not to copy every part of a national chain. You want their level of discipline, not their layers of bureaucracy. An EHR built for assisted living and memory care helps you get there.
With the right system, you can standardize documentation, protect resident data, strengthen medication management, support memory care practice, and stay ready for survey. You can give your leaders clear visibility and protect your organization when hard situations arise.
Most of all, you can show residents, families, regulators, and staff that your size does not limit your seriousness about safety and compliance. It simply makes your decisions more focused.
Conclusion
As a small or regional operator, you carry the same responsibilities as much larger organizations. An assisted living and memory care EHR does not solve every problem, but it gives you a stable foundation for compliance, risk management, and growth.
When you treat the EHR as compliance infrastructure instead of just another tool, you put your communities on the same playing field as large chains. You give your teams the structure they need, and you give yourself the visibility you deserve.
References
- Centers for Medicare & Medicaid Services. State Survey Guidance for Assisted Living Oversight.
- Office of Inspector General (OIG). Documentation Deficiencies in Residential Care Settings.
- CMS Infection Control Focus Initiative.
- National Center for Assisted Living (NCAL) Regulatory Trends Report.
- State Survey Agency Citation Analysis Reports.
- CMS Resident Assessment and Care Planning Guidance.
- Alzheimer’s Association Dementia Care Practice Recommendations.
- CMS Psychotropic Medication Oversight Guidance.
- Agency for Healthcare Research and Quality (AHRQ) Medication Safety Reports.
- Institute for Safe Medication Practices (ISMP).
- National Patient Safety Foundation Incident Reporting Standards.
- CMS Survey and Certification Process Guide.
- U.S. Department of Health and Human Services (HHS) Breach Portal Data.
- HHS Office for Civil Rights HIPAA Enforcement Actions.
- National Association of Health Care Compliance (NAHCC).
- American Health Information Management Association (AHIMA) Legal Documentation Standards.
- NCAL Growth and Risk Management Advisory.
- Insurance Industry Senior Living Claims Analysis Reports.
Disclaimer:
This article provides general information for educational purposes and does not constitute legal, regulatory, financial, or compliance advice. Assisted living and memory care regulations vary widely by state and may change without notice. Requirements related to HIPAA, cybersecurity, documentation, and electronic health records depend on your organization’s structure, payer relationships, billing methods, and operational practices.
You should consult qualified legal counsel, regulatory specialists, or state licensing authorities to determine the specific obligations that apply to your communities and to verify how the guidance in this article relates to your organization’s compliance responsibilities.