Introduction: Why visibility shapes every decision you make
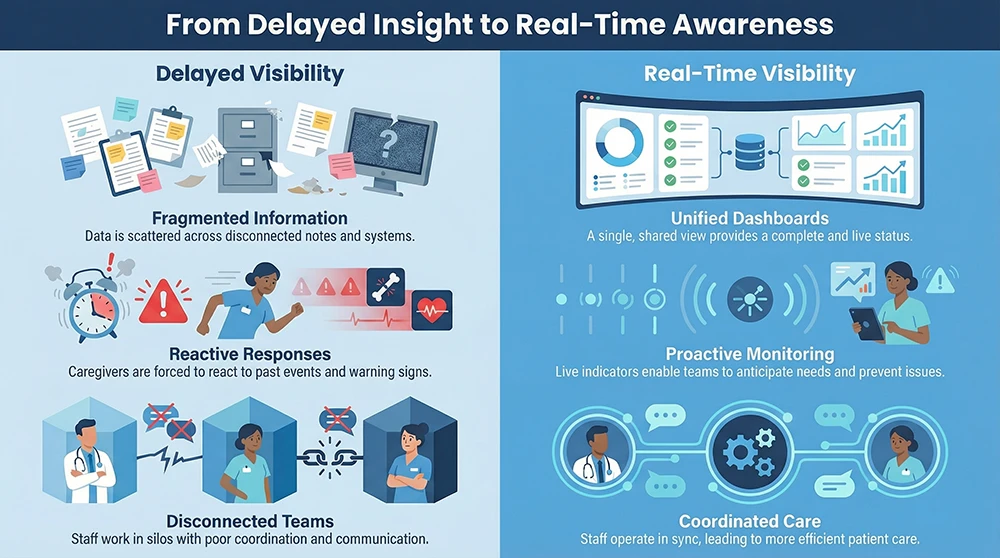
When you oversee care across dozens of assisted living and memory care communities, your biggest challenge is rarely a lack of effort from your teams. It is a lack of timely clarity. You are expected to ensure consistent clinical standards, manage staffing pressure, prepare for surveys, and respond to emerging risk, often with information that arrives hours or days too late.
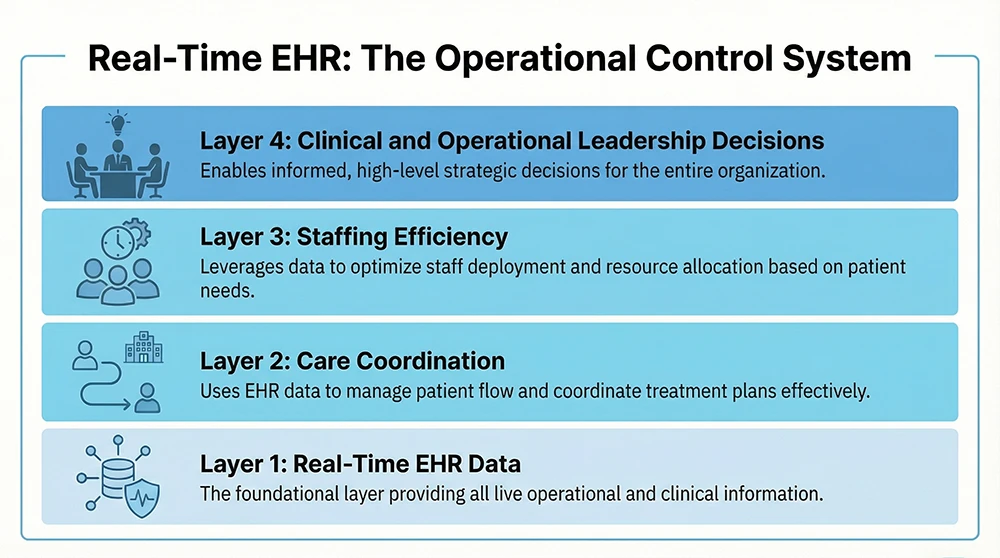
Real-time data visibility changes how you lead. An electronic health record is intended to make health information available at the point of care and across the organization, not just stored for later review (1)(2). When that information updates as care happens, you move from reacting to problems after the fact to guiding care and staffing decisions while they still matter.
What real-time data visibility means in assisted living and memory care
Real time is about when decisions happen
In your environment, real-time visibility means staff document care as it occurs, and the system reflects those updates immediately. You do not have to wait for the end of a shift to learn that a resident needed more assistance, that behaviors escalated, or that care tasks were missed. The information is visible while there is still time to respond (1)(10).
This matters because assisted living and memory care rely on constant handoffs. When documentation lags, each handoff becomes a reconstruction exercise. When documentation is current, handoffs become confirmation.
Why memory care raises the stakes
Memory care intensifies the need for visibility. Residents may not be able to describe pain, discomfort, or emotional distress. Subtle changes in behavior or routine are often the first signs that something is wrong. National guidance on older adult health emphasizes early recognition of change as a key factor in preventing decline (3).
When those observations are documented in real time and visible to supervisors and clinical leaders, care plans can be adjusted sooner, and teams stay aligned.
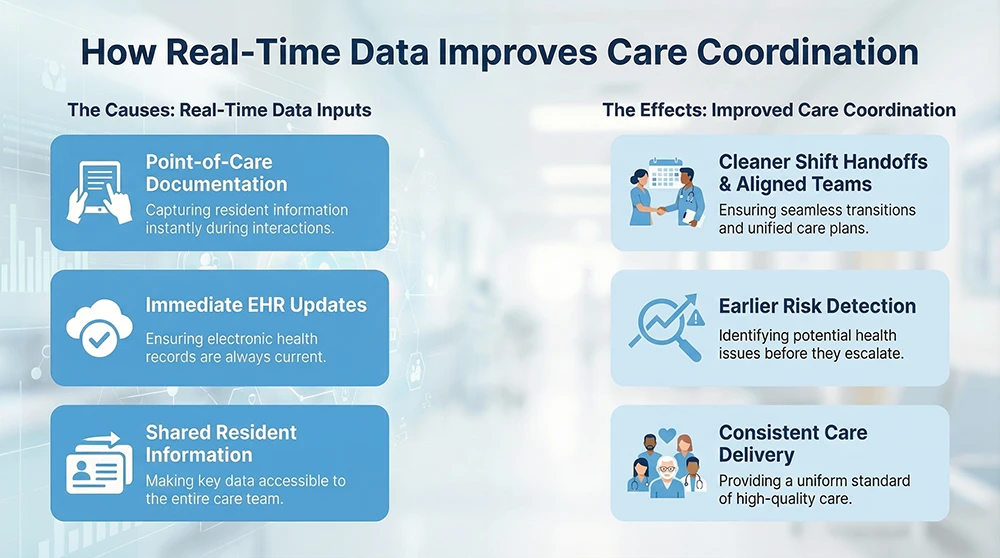
How real-time visibility strengthens care coordination
Cleaner handoffs and fewer missed details
Care coordination depends on shared understanding. AHRQ defines it as organizing activities and sharing information so care meets patient needs over time (3)(9). In practice, this means the next caregiver should know exactly what happened before they arrived.
When your EHR reflects current information, handoffs improve. Staff are no longer relying on memory or verbal summaries alone. You see what was completed, what changed, and what still needs attention. Across many communities, this consistency reduces variability and lowers the risk that important details fall through the cracks.
Earlier recognition of risk patterns
Most adverse events are preceded by small signals. A resident needs a little more help. Behaviors become more frequent. PRN medications are less effective. When these details are documented but buried in delayed notes, they are easy to miss.
Real-time visibility allows you and your leaders to see patterns forming. That supports earlier intervention, whether that means a clinical review, a care plan update, or additional staff support. This proactive approach aligns with national care coordination frameworks that emphasize anticipation rather than reaction (3)(9).
Consistent care standards across many buildings
Operating at scale introduces variation. Even with shared policies, practice can drift from one building to another. Assisted living regulation is largely state-based, which adds complexity for multi-state operators (15)(16).
When documentation and care delivery are visible in real time, you can see where standards are being met and where they are not. Coaching becomes more specific, and expectations become clearer. Over time, this reduces unwarranted variation and supports more predictable resident outcomes.
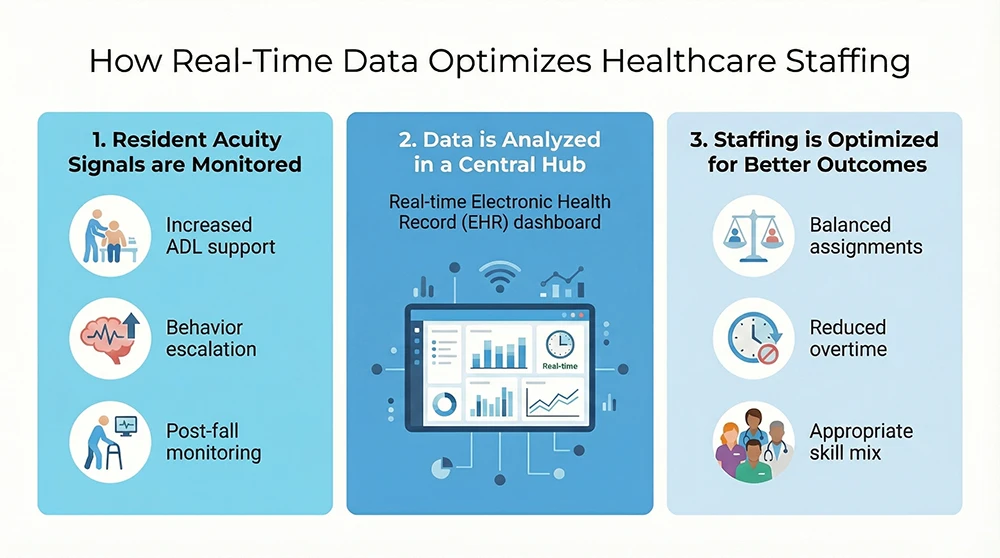
How real-time visibility improves staffing efficiency
Staffing decisions tied to acuity, not assumptions
Traditional staffing models often rely on census or historical patterns. Those approaches miss daily fluctuations in resident need. An EHR is designed to capture clinical information over time, including changes that affect workload (2)(8).
When you can see current assistance levels, monitoring needs, and care complexity, staffing decisions become more precise. You are not guessing which shift will be heavy. You are responding to what residents actually require that day.
Fairer workloads and less reactive overtime
Uneven workload is a common driver of burnout. When staff consistently carry heavier assignments without support, frustration builds. National data from the CDC shows high levels of burnout among health workers, with long hours and workload stress identified as major contributors (4)(5).
Real-time visibility helps you redistribute support before problems escalate. Supervisors can see where workload is spiking and adjust assignments or bring in help earlier. Over time, this reduces emergency overtime and supports a more sustainable staffing rhythm.
More time spent on care, less time chasing information
Caregivers lose time when information is hard to find or outdated. Modern EHR guidance emphasizes timely documentation and retrieval to support care delivery (1)(10).
When staff can quickly see current care instructions and document at the point of service, they spend less time clarifying expectations and more time with residents. That efficiency benefits both care quality and morale.
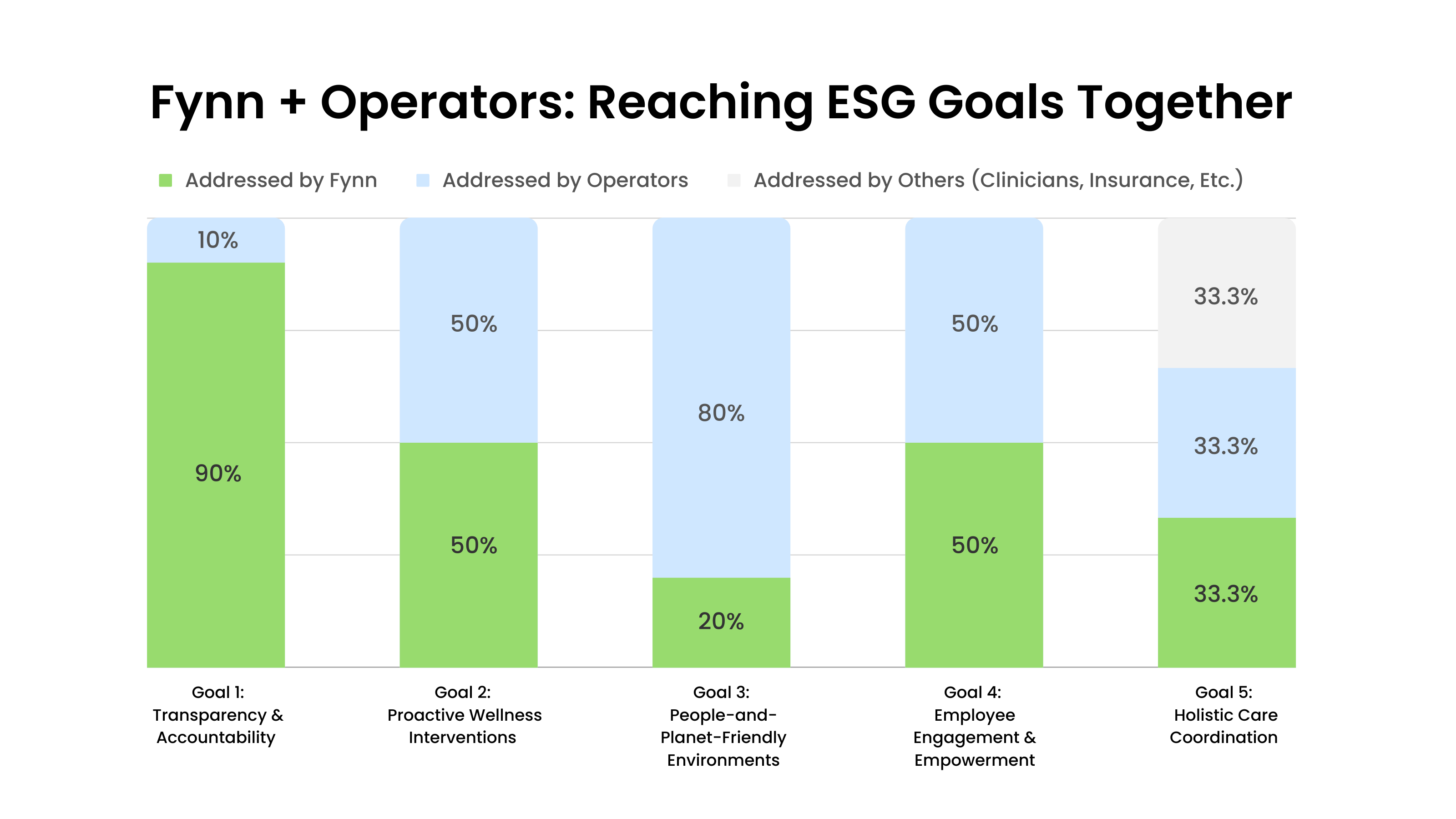
For organizations evaluating how technology supports this level of visibility, Fynn’s EHR platform for assisted living and memory care illustrates how real-time documentation and enterprise access can support both care coordination and staffing decisions.
What changes when you manage at the enterprise level
Less chasing updates, more directing action
When you oversee 40 or more communities, updates often arrive through multiple channels. That fragments your attention and slows response time.
Enterprise EHR visibility allows you to review key signals across the portfolio in one place. You can identify where risk is rising, where documentation is lagging, and where staffing pressure is building. Instead of collecting updates, you direct action.
Stronger compliance posture through timely records
Documentation is central to regulatory oversight. CMS and HHS guidance emphasizes documentation integrity, accuracy, and timeliness (17). Late or incomplete records increase organizational risk during surveys and investigations.
Real-time documentation supports compliance by showing that care was planned, delivered, and evaluated as required. When records are current, leadership can respond to survey requests with confidence rather than reconstruction.
Clearer access control supports security obligations
EHRs contain sensitive information, and HIPAA’s Security Rule requires safeguards to protect electronic health information (19)(20). Visibility paired with role-based access and audit trails helps ensure staff see what they need, and only what they need.
This clarity reduces both privacy risk and operational confusion.
Common obstacles and how to address them
Adoption challenges often appear as data problems. When staff delay documentation, dashboards lose credibility. Addressing this requires workflow-aligned training, clear expectations, and supervisor coaching. AHRQ implementation guidance emphasizes structured change management and reinforcement, not one-time training (21)(22).
Another risk is alert overload. Real-time systems should highlight what requires action, not everything that changes. Role-based views help protect focus and prevent important signals from being buried.
Standardization is also essential. Enterprise visibility only works when communities document the same concepts in consistent ways. Shared definitions and documentation practices make comparisons meaningful and support coordinated action (3)(9).
Conclusion: Visibility supports steadier leadership
When you can see resident needs and staff workload as they shift, you coordinate care with fewer delays and fewer surprises. Real-time EHR visibility supports earlier risk recognition, clearer handoffs, and staffing decisions that reflect actual demand. For leaders responsible for care quality across many communities, that visibility becomes a daily operational advantage rather than a reporting exercise (3)(4)(5)(6).
References
- Office of the National Coordinator for Health IT. What Are Electronic Health Records (EHRs)?
- Centers for Medicare & Medicaid Services. Electronic Health Records.
- Agency for Healthcare Research and Quality. Care Coordination Measures Atlas.
- Centers for Disease Control and Prevention. Health Worker Burnout.
- CDC NIOSH. Risk Factors for Stress and Burnout in Healthcare Workers.
- U.S. Bureau of Labor Statistics. Nursing Assistants Occupational Data.
- U.S. Bureau of Labor Statistics. Occupational Outlook Handbook.
- National Library of Medicine. Electronic Health Records Overview.
- AHRQ. Care Coordination Measurement Framework.
- ONC. Health IT Playbook.
- Congressional Research Service. Overview of Assisted Living Facilities.
- AHCA/NCAL. State Regulatory Resources.
- CMS. Documentation Integrity Guidance.
- HHS Office for Civil Rights. HIPAA Security Rule.
- HHS. Summary of HIPAA Security Rule.
- AHRQ TeamSTEPPS. Implementation Change Management.
- AHRQ TeamSTEPPS. Teaching Change Management.
Compliance Disclaimer:
This article provides general information and is not legal advice. State-specific regulations vary.
Disclaimer:
This article provides general information for educational purposes and does not constitute legal, regulatory, financial, or compliance advice. Assisted living and memory care regulations vary widely by state and may change without notice. Requirements related to HIPAA, cybersecurity, documentation, and electronic health records depend on your organization’s structure, payer relationships, billing methods, and operational practices.
You should consult qualified legal counsel, regulatory specialists, or state licensing authorities to determine the specific obligations that apply to your communities and to verify how the guidance in this article relates to your organization’s compliance responsibilities.






.jpeg)