Corporate health and wellness directors in assisted living and memory care balance busy schedules and constant oversight needs. You guide teams, review records, and support residents who rely on consistent and safe care. When a state reviewer or a CMS contractor arrives, the story inside your electronic health records becomes the foundation of the entire audit. The difference between a smooth visit and a penalty often comes down to how complete, clear, and organized your documentation is. (1)(2)(11)(12)
Why Documentation Has Become the Deciding Factor

Across many states, surveyors rely on documentation to understand how well residents are assessed, supported, and monitored. Assisted living rules vary, yet reviewers tend to follow similar principles. They look for clear records that connect assessments to care plans and care plans to daily notes. (1)(2)(12)
Federal auditors point to insufficient or missing documentation as one of the most common reasons for improper payment findings. (5)(6)(7) Services may be legitimate, but if the documentation is incomplete, reviewers may count them as unsupported. CMS guidance states that if the record does not show what occurred, reviewers may assume the service did not happen. (4)
If you work with Medicaid, managed care groups, or clinical partners such as hospice or therapy providers, missing documentation can also lead to separate penalties or delays. (5)(6)(12) In this environment, your EHR becomes more than a charting tool. It becomes your organization’s main defense during any audit.
What Reviewers Expect to Find in Your Records
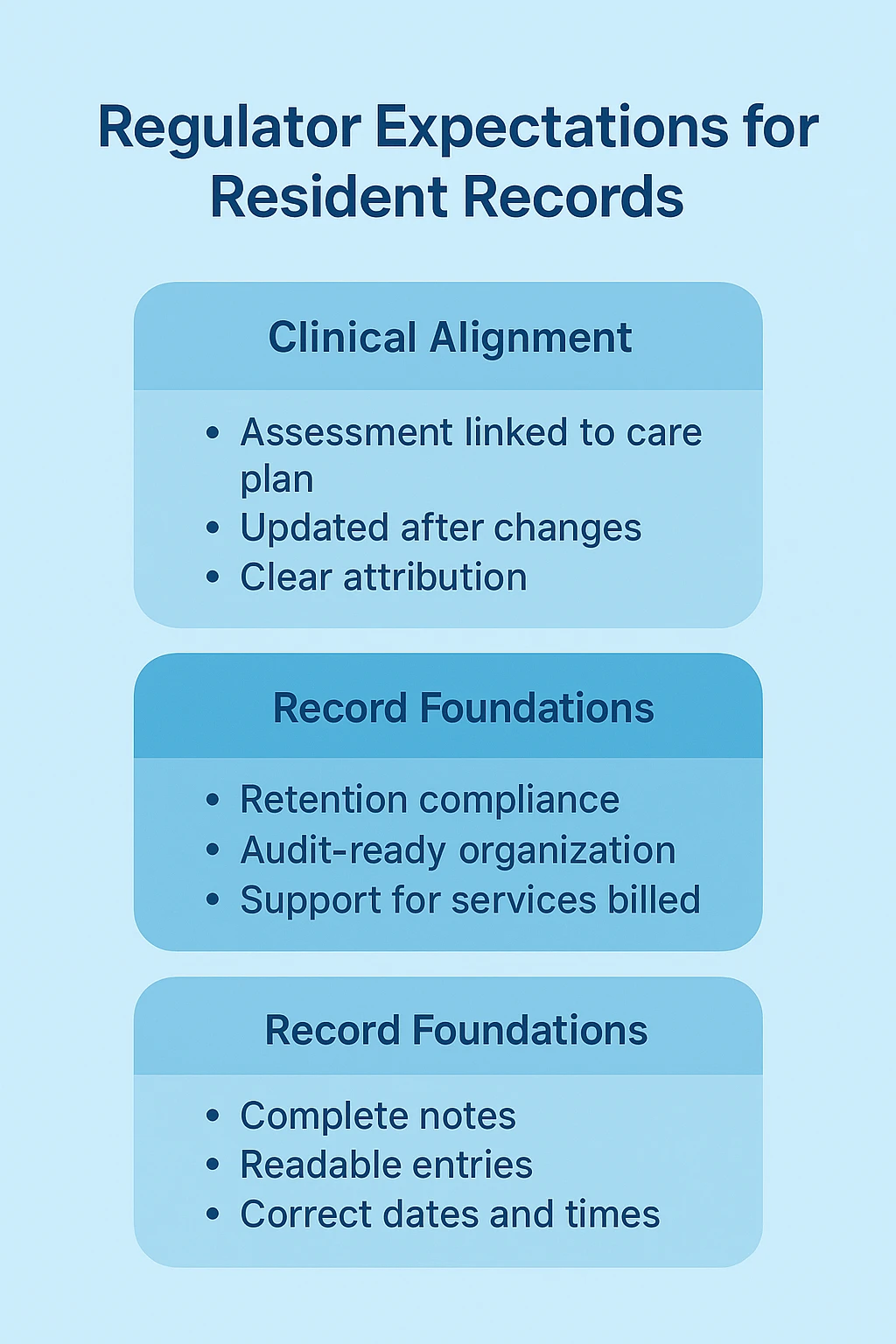
Although each state has its own rules, reviewers usually expect records that are easy to read, correctly attributed, and updated in a timely manner. Notes should include dates, times, and staff signatures. (2)(4) Care plans should reflect the most recent assessments and demonstrate a clear connection between identified needs and the services your teams provide. (1)(2)(4)
CMS also expects medical records to be kept for specific retention periods, often at least seven years. (3) Well-organized records help reviewers understand the resident’s experience and help your staff respond confidently during an audit.
EHR Features That Help Prevent Penalties

Assessment and Care Plan Tools That Follow Common Regulatory Expectations
In many audits, findings occur because assessments and care plans do not match or were not updated after a change in condition. (1)(2)(12) A well-designed EHR can guide your teams through each step. When templates reflect ADLs, cognitive changes, fall risks, chronic conditions, and behavioral patterns, staff are less likely to miss required information.
When assessments connect naturally to service plans, reviewers can see how your teams evaluated the resident and how the care plan was developed. (2)(4) Version histories help show when changes occurred and why adjustments were made. This gives your records a clear timeline and helps you demonstrate consistent clinical leadership.
Here’s where your corporate clinical systems strategy can shine: by selecting an EHR such as the Fynn Platform, you equip your teams with workflows that mirror what surveyors expect to see. This alignment elevates your documentation from “good enough” to defensible.
Guardrails That Reduce Missing or Incomplete Information
Many penalties trace back to incomplete documentation. Missing times, unsigned orders, or lack of rationale for care decisions can raise concerns quickly. (4)(5) EHRs with required fields prevent staff from closing notes without finishing essential parts. Conditional prompts can help team members document follow-up steps, such as resident response after a PRN medication. (2)(4)
These tools support your teams in real time. Corrections after the fact become less common, and your communities build stronger habits that hold up well during reviews.
Medication Records That Hold Up Under Review
Medication documentation receives close attention during surveys. Reviewers often look for clear evidence of when medications were given, whether refusals were documented, and whether staff recorded clinical reasons for high risk or PRN medications. (1)(2)(4)(11)
An eMAR that stays fully aligned with active orders helps reduce errors. When timestamps, staff credentials, and notes are included for each dose, the resulting medication history becomes easier to follow and defend. For memory care, where behaviors and health changes often relate to medications, this clarity is especially valuable.
Incident and Change in Condition Documentation That Tells a Complete Story
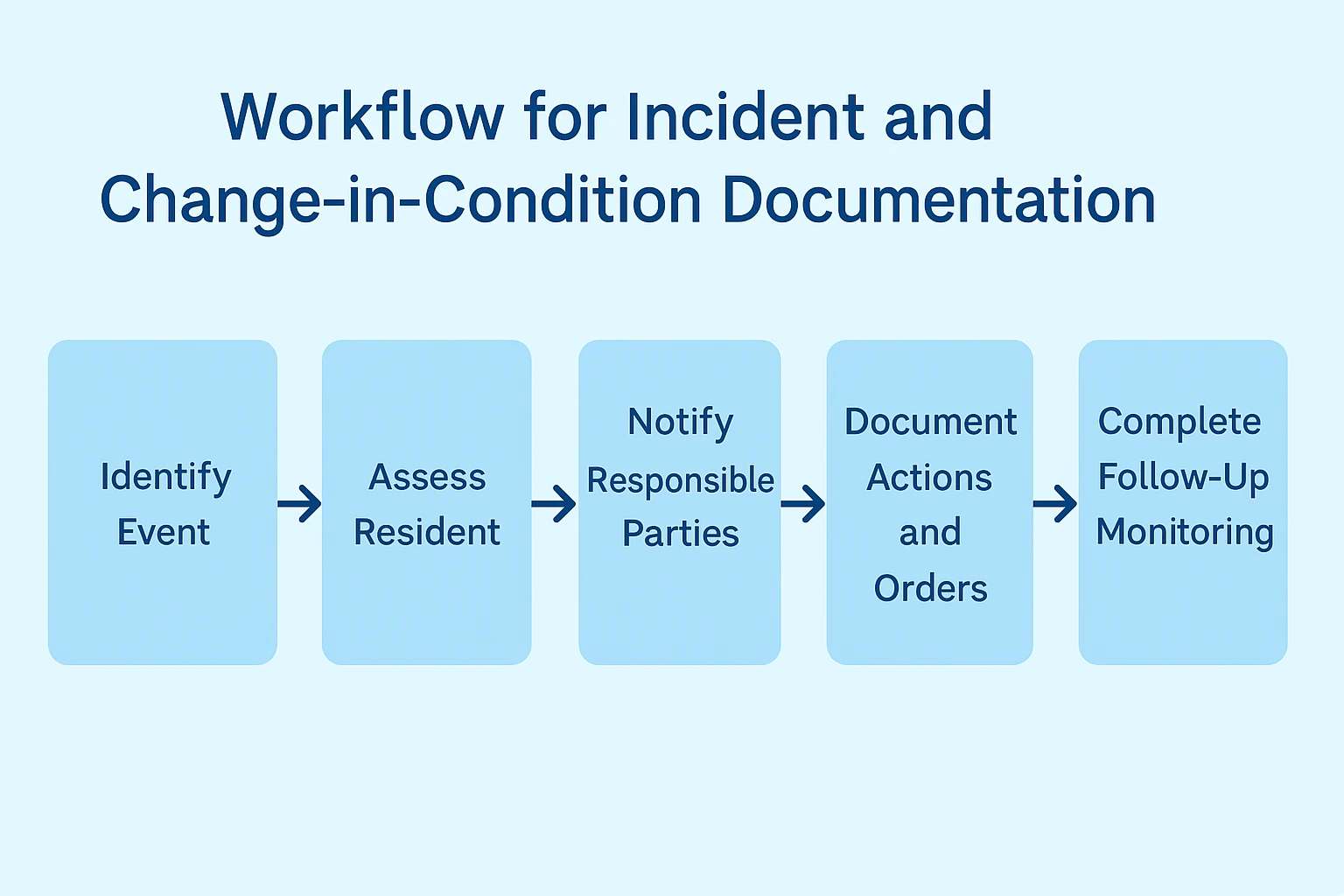
Reviewers study how your community responds to falls, injuries, acute symptoms, and other significant events. They want to see that staff assessed the situation promptly, notified the right people, followed provider orders, and monitored the resident afterward. (1)(2)(11)(12)
Strong EHR workflows help your teams capture what happened, who responded, what actions were taken, and how the resident was monitored. This helps create a clear timeline that matches regulatory expectations and reduces gaps that might lead to citations.
Audit Trails That Protect Record Integrity
To meet HIPAA requirements, your EHR must show who accessed a record, what they viewed, and what they changed. (8)(9)(10) Systems that produce complete audit logs help you respond confidently if questions arise about privacy or record accuracy. Alerts for unusual access patterns help your organization protect residents and document that you monitored for risks. (8)(9)(10)
Corporate Dashboards That Improve Oversight
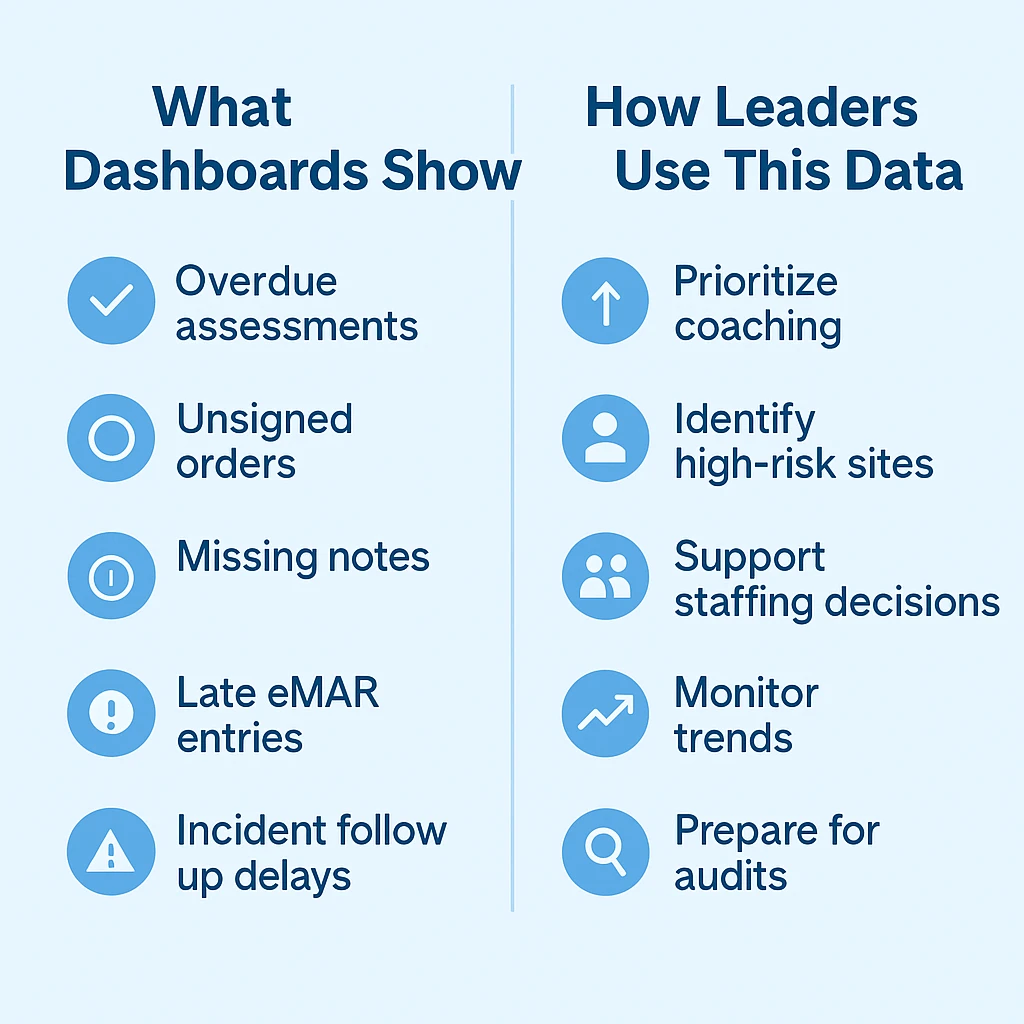
Strong oversight reduces audit surprises. Many EHRs include dashboards that show overdue assessments, unsigned orders, missing progress notes, or late eMAR entries. (1)(11)(12)(18) You can review each community’s trends, support teams that need coaching, and close gaps before a reviewer notices them.
These tools help you work more proactively, especially when you support multiple buildings with different staffing patterns and clinical needs.
Tools That Support Record Retention and Survey Readiness
During an audit, the ability to produce complete records quickly matters. Systems that generate unified record packets can help your staff respond without searching through separate files. (3)(4)(11) When documents appear in a clean and logical structure, reviewers can follow the resident’s history more easily and your team feels more confident throughout the process.
Communication Tools That Strengthen Interdisciplinary Work
Surveyors often look for evidence of communication among nurses, caregivers, physicians, therapists, and family members. (1)(2)(11)(12) Secure messaging, handoff tools, and interdisciplinary notes help show that your teams shared important information at the right times. Clear communication records help demonstrate continuity of care and reduce the risk of findings related to miscommunication.
How Corporate Nursing Leaders Bring Everything Together
Technology alone does not protect your organization. NIST, HIPAA, and CMS guidance point to the need for policies, training, monitoring, and risk assessments. (5)(8)(9)(26) Your role is to make sure the system supports your policies and your staff know how to use it correctly.
Many leaders create a regular review process that includes mock audits, template updates, and audits of documentation accuracy. (1)(2)(5)(11) When you treat your EHR as a living part of your compliance program, you give your communities the structure they need to prevent errors and respond well to reviews.
References
- Centers for Medicare & Medicaid Services (CMS). Long-Term Care Facilities – Conditions of Participation and survey basis for nursing facilities.
- CMS. State Operations Manual Appendix PP – Guidance to Surveyors for Long-Term Care Facilities.
- CMS. Medical Record Maintenance & Access Requirements (MLN Fact Sheet).
- CMS. Complying with Medical Record Documentation Requirements (MLN Educational Tool).
- CMS. Fiscal Year 2024 Improper Payments Fact Sheet.
- U.S. Government Accountability Office (GAO). Medicaid Managed Care: Improper Payment Estimate.
- McKnight’s Long-Term Care News. Coverage of Medicare improper payment trends.
- U.S. Department of Health & Human Services (HHS), Office for Civil Rights. HIPAA Security Rule Overview.
- National Institute of Standards & Technology (NIST). Special Publication 800-66 Revision 2.
- HIPAA Journal. HIPAA Audit Checklist and Audit Log Requirements.
- CMS. Nursing Home Enforcement Overview.
- Texas Health and Human Services Commission. Long-Term Care Facility Regulation Fact Sheet.
- (Entry for compliance dashboards and monitoring trends)
- NIST. Framework for Improving Critical Infrastructure Cybersecurity (related to risk assessments)
Disclaimer:
This article provides general information for educational purposes and does not constitute legal, regulatory, financial, or compliance advice. Assisted living and memory care regulations vary widely by state and may change without notice. Requirements related to HIPAA, cybersecurity, documentation, and electronic health records depend on your organization’s structure, payer relationships, billing methods, and operational practices.
You should consult qualified legal counsel, regulatory specialists, or state licensing authorities to determine the specific obligations that apply to your communities and to verify how the guidance in this article relates to your organization’s compliance responsibilities.